Empowering Disability Communities through Inclusive Transfemoral Prosthesis Co-Design with a Local SME in Indonesia
DOI:
https://doi.org/10.12928/spekta.v6i1.13091Keywords:
Amputee Mobility Predictor with Prosthesis (AMPPRO), Disabilities, Locomotor Capabilities Index (LCI), Product Design, Prosthetic EvaluationAbstract
Background: Lower-limb loss poses significant challenges to mobility, employability, and social participation for many individuals in low- and middle-income countries. In Indonesia, the high cost of imported prosthetics has prompted community-based small enterprises to produce low-cost transfemoral devices.
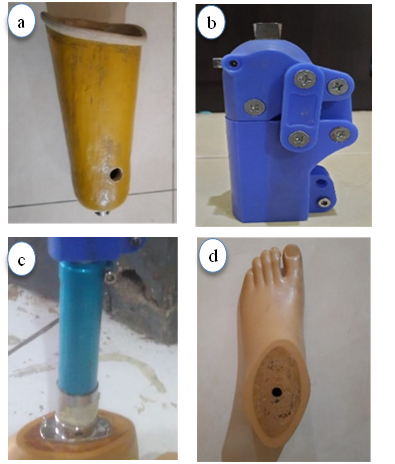
Contribution: This study contributes to support a local prosthetics workshop (Independent Disabled Creativity Foundation/IDCF) by integrating user feedback and basic functional assessments to guide improvements to a transfemoral prosthesis prototype.
Method: Seven transfemoral amputees completed the Locomotor Ability Index (LCI), then performed standing, walking, and stair climbing tasks assessed by the Amputee Mobility Predictor with Prosthesis (AMPPRO), Rating of Perceived Discomfort (RPD) questionnaire, and Post-test Interview with improvement concepts using the SCAMPER (Substitute, Combine, Adapt, Modify, Put to Other uses, Eliminate, Rearrange) creativity method.
Results: Participants achieved independent ambulation (mean LCI = 51.00 ± 5.10; AMPPRO = 42.29 ± 3.15, K3–K4 classification). Common discomfort was reported in the amputated thigh, sound-side thigh, and ankle. Design adjustments were collaboratively proposed, including socket fit improvement, knee joint reinforcement, and coupler alignment.
Conclusion: This study highlights the value of structured user feedback in guiding local prosthetic refinement. It demonstrates how participatory methods can support inclusive design and technical strengthening for community-based production.
References
R. I. Emeilia, N. Novalia, A. Muntazah, and R. Andhikasari, “Strategi Komunikasi Dinas Sosial Tangerang Selatan Dalam Program Pelayanan Penyaluran Alat Bantu Disabilitas,” Innov. J. of Social Science Research, 2024, [Online]. Available: http://j-innovative.org/index.php/Innovative/article/view/13350.
L. Calabrese, M. Maffoni, V. Torlaschi, and A. Pierobon, “What Is Hidden behind Amputation? Quanti-Qualitative Systematic Review on Psychological Adjustment and Quality of Life in Lower Limb Amputees for Non-Traumatic Reasons,” Healthcare, vol. 11, no. 11, p. 1661, Jun. 2023, doi: 10.3390/healthcare11111661.
L. Coffey, P. Gallagher, and D. Desmond, “Goal Pursuit and Goal Adjustment as Predictors of Disability and Quality of Life Among Individuals With a Lower Limb Amputation: A Prospective Study,” Arch. Phys. Med. Rehabil., vol. 95, no. 2, pp. 244–252, Feb. 2014, doi: 10.1016/j.apmr.2013.08.011.
K. Demet, N. Martinet, F. Guillemin, J. Paysant, And J.-M. Andre, “Health related quality of life and related factors in 539 persons with amputation of upper and lower limb,” Disabil. Rehabil., vol. 25, no. 9, pp. 480–486, Jan. 2003, doi: 10.1080/0963828031000090434.
M. de Andrade Fonseca, A. G. Cordeiro Matias, M. de Lourdes de Freitas Gomes, and M. Almeida Matos, “Impact of Lower Limb Fractures on the Quality of Life,” Ortop. Traumatol. Rehabil., vol. 21, no. 1, pp. 33–40, Feb. 2019, doi: 10.5604/01.3001.0013.1078.
S. Love, “Predicting Walking Ability and Prosthetic Candidacy Following Lower Extremity Amputation: Systematic Review, Treatment Pathway and Algorithm,” University of St. Augustine for Health Sciences, 2016. https://soar.usa.edu/dissertations/17/
P. Shankar, V. S. Grewal, S. Agrawal, and S. V. Nair, “A study on quality of life among lower limb amputees at a tertiary prosthetic rehabilitation center,” Med. J. Armed Forces India, vol. 76, no. 1, pp. 89–94, Jan. 2020, doi: 10.1016/j.mjafi.2019.02.008.
W. H. Organization, “World report on disability,” World Rep. Disabil., 2011, [Online]. Available: https://pesquisa.bvsalud.org/portal/resource/pt/biblio-1052751.
W. H. Organization, “World Bank.(2011). World report on disability 2011,” World Health Organization. 2023. https://iris.who.int/
N. Arifin, N. Abu Osman, S. Ali, and W. Wan Abas, “The effects of prosthetic foot type and visual alteration on postural steadiness in below-knee amputees,” Biomed. Eng. Online, vol. 13, no. 1, p. 23, 2014, doi: 10.1186/1475-925X-13-23.
R. Gailey, “Review of secondary physical conditions associated with lower-limb amputation and long-term prosthesis use,” J. Rehabil. Res. Dev., vol. 45, no. 1, pp. 15–30, Dec. 2008, doi: 10.1682/JRRD.2006.11.0147.
A. D. Knight, C. L. Dearth, and B. D. Hendershot, “Deleterious Musculoskeletal Conditions Secondary to Lower Limb Loss: Considerations for Prosthesis-Related Factors,” Adv. Wound Care, vol. 10, no. 12, pp. 671–684, Dec. 2021, doi: 10.1089/wound.2019.1079.
C. Quintero-Quiroz and V. Z. Perez, “Materials for lower limb prosthetic and orthotic interfaces and sockets: Evolution and associated skin problems,” Rev. la Fac. Med., vol. 67, no. 1, pp. 117–125, Jan. 2019, doi: 10.15446/revfacmed.v67n1.64470.
I. Fagioli, “Advancements and Challenges in the Development of Robotic Lower Limb Prostheses: A Systematic Review,” IEEE Trans. Med. Robot. Bionics, vol. 6, no. 4, pp. 1409–1422, Nov. 2024, doi: 10.1109/TMRB.2024.3464126.
S. Fatone, “Comparison of Ischial Containment and Subischial Sockets on Comfort, Function, Quality of Life, and Satisfaction With Device in Persons With Unilateral Transfemoral Amputation: A Randomized Crossover Trial,” Arch. Phys. Med. Rehabil., vol. 102, no. 11, pp. 2063-2073.e2, Nov. 2021, doi: 10.1016/j.apmr.2021.05.016.
S.-T. Ko, F. Asplund, and B. Zeybek, “A Scoping Review of Pressure Measurements in Prosthetic Sockets of Transfemoral Amputees during Ambulation: Key Considerations for Sensor Design,” Sensors, vol. 21, no. 15, p. 5016, Jul. 2021, doi: 10.3390/s21155016.
B. Tyagi, “Fabrication of transfemoral prosthesis utilizing additive manufacturing and reverse engineering: a scoping review,” Int. J. Interact. Des. Manuf., vol. 18, no. 6, pp. 3613–3631, Aug. 2024, doi: 10.1007/s12008-024-01974-0.
S. Turner, A. Belsi, and A. H. McGregor, “Issues faced by people with amputation(s) during lower limb prosthetic rehabilitation: A thematic analysis,” Prosthetics Orthot. Int., vol. 46, no. 1, pp. 61–67, Feb. 2022, doi: 10.1097/PXR.0000000000000070.
M. E. Matsumoto, J. Cave, and J. Shaffer, “Innovations in Amputation Rehabilitation and Prosthetic Design,” Phys. Med. Rehabil. Clin. N. Am., vol. 35, no. 4, pp. 879–896, Nov. 2024, doi: 10.1016/j.pmr.2024.06.008.
D. Suprayogi, Perbedaan Keseimbangan Dinamis Penggunaan Transfemoral Prosthesis dengan Axillary Crutch pada Pasien Pascaamputasi Transfemoral. books.google.com, 2022. https://id.scribd.com/document/817877343/repo-file-206631-20230919-112709
G. E. Prinanda, Studi Geometri dan Finite Element Analysis pada Telapak Kaki Asli dan Buatan. dspace.uii.ac.id, 2023. https://dspace.uii.ac.id/handle/123456789/46677
C. Gauthier-Gagnon and M. C. Grise, “Tools to measure outcome of people with a lower limb amputation: Update on the PPA and LCI,” JPO J. Prosthetics and Orthotics, 2006, [Online]. Available: https://journals.lww.com/jpojournal/fulltext/2006/01001/tools_to_measure_outcome_of_people_with_a_lower.7.aspx.
A. Ranker, C. Gutenbrunner, I. Eckhardt, A. Giordano, H. Burger, and F. Franchignoni, “Rasch validation and comparison of the German versions of the Locomotor Capabilities Index-5 and Prosthetic Mobility Questionnaire 2.0 in lower-limb prosthesis users,” Int. J. Rehabil. Res., vol. 44, no. 3, pp. 233–240, Sep. 2021, doi: 10.1097/MRR.0000000000000478.
R. S. Gailey, “The Amputee Mobility Predictor: An instrument to assess determinants of the lower-limb amputee’s ability to ambulate,” Arch. Phys. Med. Rehabil., vol. 83, no. 5, pp. 613–627, May 2002, doi: 10.1053/apmr.2002.32309.
S. JS, “The validity and reliability of a rating scale of perceived exertion,” Med Sci Sports. cir.nii.ac.jp, 1973, [Online]. Available: https://cir.nii.ac.jp/crid/1570009750090505344.
S. Sadeghian, A. Uhde, and M. Hassenzahl, “The Soul of Work: Evaluation of Job Meaningfulness and Accountability in Human-AI Collaboration,” Proceedings of the ACM Hum. Computer Interaction, 2024, doi: 10.1145/3637407.
J. R. Wilson and S. Sharples, Evaluation of human work. books.google.com, 2015.
O. Serrat, “The SCAMPER Technique,” in Knowledge Solutions, Singapore: Springer Singapore, 2017, pp. 311–314. Doi: 10.1007/978-981-10-0983-9_33
G. Tao, G. Charm, K. Kabacińska, W. C. Miller, and J. M. Robillard, “Evaluation Tools for Assistive Technologies: A Scoping Review,” Arch. Phys. Med. Rehabil., vol. 101, no. 6, pp. 1025–1040, Jun. 2020, doi: 10.1016/j.apmr.2020.01.008.
G. M. Berke, “Comparison of satisfaction with current prosthetic care in veterans and servicemembers from Vietnam and OIF/OEF conflicts with major traumatic limb loss,” J. Rehabil. Res. Dev., vol. 47, no. 4, p. 361, 2010, doi: 10.1682/JRRD.2009.12.0193.
T. Schmalz, M. Bellmann, E. Proebsting, and S. Blumentritt, “Effects of Adaptation to a Functionally New Prosthetic Lower-Limb Component,” JPO J. Prosthetics Orthot., vol. 26, no. 3, pp. 134–143, Jul. 2014, doi: 10.1097/JPO.0000000000000028.
P. Gallagher and M. MacLachlan, “Adjustment to an artificial limb: a qualitative perspective,” J. Health Psychol., 2001, doi: 10.1177/135910530100600107.
N. Arshad, H. Khan, K. U. Rehman, and M. A. Sadiq, “Frequency of phantom limb pain, limb sensation and stump pain among amputees,” Int J Health Sciences. researchgate.net, 2023, [Online]. Available: https://www.researchgate.net/profile/Naveed-Arshad/publication/367326902_Frequency_of_phantom_limb_pain_limb_sensation_and_stump_pain_among_amputees/links/63cc0d0ee922c50e99b1f88c/Frequency-of-phantom-limb-pain-limb-sensation-and-stump-pain-among-amputees.
R. W. Davis, “Phantom sensation, phantom pain, and stump pain,” Arch. Phys. Med. Rehabil., 1993, [Online]. Available: https://www.archives-pmr.org/article/0003-9993(93)90388-Q/fulltext.
C. Lake, “The evolution of upper limb prosthetic socket design,” JPO J. Prosthetics Orthot., 2008, [Online]. Available: https://journals.lww.com/jpojournal/fulltext/2008/07000/The_Evolution_of_Upper_Limb_Prosthetic_Socket.5.aspx.
C. Curtze, A. L. Hof, K. Postema, and B. Otten, “Staying in dynamic balance on a prosthetic limb: A leg to stand on?,” Med. Eng. Phys., vol. 38, no. 6, pp. 576–580, Jun. 2016, doi: 10.1016/j.medengphy.2016.02.013.
R. N. Stauffer and E. Y. S. Chao, “Force and motion analysis of the normal, diseased, and prosthetic ankle joint,” Clin. Orthop. Relat Res, 1977, [Online]. Available: https://journals.lww.com/corr/citation/1977/09000/force_and_motion_analysis_of_the_normal,_diseased,.27.aspx.
A. S. Aruin, J. J. Nicholas, and M. L. Latash, “Anticipatory postural adjustments during standing in below-the-knee amputees,” Clin. Biomech., 1997, [Online]. Available: https://www.sciencedirect.com/science/article/pii/S0268003396000538.
E. Lathouwers, “Therapeutic benefits of lower limb prostheses: a systematic review,” J. Neuroeng. Rehabil., vol. 20, no. 1, p. 4, Jan. 2023, doi: 10.1186/s12984-023-01128-5.
A. Seireg and R. J. Arvikar, “The prediction of muscular load sharing and joint forces in the lower extremities during walking,” J. Biomech., 1975, [Online]. Available: https://www.sciencedirect.com/science/article/pii/0021929075900895.
J. Andrysek, S. Klejman, R. Torres-Moreno, W. Heim, B. Steinnagel, and S. Glasford, “Mobility function of a prosthetic knee joint with an automatic stance phase lock,” Prosthetics Orthot. Int., vol. 35, no. 2, pp. 163–170, Jun. 2011, doi: 10.1177/0309364611408495.
K. Wang, “Design and Evaluation of a Smooth-Locking-Based Customizable Prosthetic Knee Joint,” J. Mech. Robot., vol. 16, no. 4, Apr. 2024, doi: 10.1115/1.4062498.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Khoirul Muslim, Dias Nuryamsi, Rifko Rahmat Kurnianto, Sandro Mihradi

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Authors who publish with SPEKTA (Jurnal Pengabdian Kepada Masyarakat: Teknologi dan Aplikasi) agree to the following terms:
- Authors retain copyright and grant the journal the right of first publication with the work simultaneously licensed under a Creative Commons Attribution License (CC BY-SA 4.0) that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.












