The Practices of Artificial Intelligence Techniques and Their Worth in the Confrontation of COVID-19 Pandemic: A Literature Review
DOI:
https://doi.org/10.12928/mf.v4i1.5691Keywords:
Artificial Intelligence, COVID-19, SARS-CoV-2, Vaccines, Machine Learning, Deep LearningAbstract
Today, the medical society is living in the era of artificial intelligence, which is developed and becomes more famous thanks to the coronavirus disease of 2019 (COVID-19) pandemic, which has given the space for artificial intelligence to appear more influential in analyzing medical data and providing very accurate results. This science has deservedly been able to achieve an excellent and vital position among healthcare workers, and it has become a necessary element of their work because of its a great potential for practical decision-making. The prospects of using intelligent systems in the medical field are deemed essential in the health division due to their ability to analyze big data and give exact results, aiming to improve the health of citizens and save their lives. In this article, a set of important information about the vital role of artificial intelligence in the medical field is highlighted. In addition, how this science does manage to confront SARS‐CoV‐2 by highlighting a set of investigations and analyses in predicting the spread of the virus, tracking infections, and diagnosis of cases through chest x-ray images of COVID-19 patients. The database of this article covered more than 40 studies between 2020 and 2021 and investigated the effects of utilizing artificial intelligence techniques in analyzing SARS‐CoV‐2 data. These studies are gathered from PubMed, NCBI, google scholar, Medrxiv, and other sites. This article includes a plethora of information about artificial intelligence and SARS‐CoV‐2. The findings confirm that artificial intelligence has a significant role in the healthcare domain, and it is advised to utilize its applications in the decision-making method.
References
Turing A. M., "Computing Machinery and Intelligence, Mind, vol. lix, no.236, pp:433–460, October 1950. https://doi.org/10.1093/mind/LIX.236.433
Rajaraman V., “John McCarthy – Father of Artificial Intelligence,” Asia Pacific Mathematics Newsletter, vol.4, no.3, pp:15-20, July 2014.
Jin C, Chen W, Cao Y, Xu Z, Tan Z, Zhang X., et al., “Development and evaluation of an artificial intelligence system for COVID-19 diagnosis,” Nature Communications, vol.11, article number: 5088, pp:1-14, October 2020. https://doi.org/10.1038/s41467-020-18685-1
Jakhar P., Coronavirus: China's tech fights back (2020), Retrieved from BBC Monitoring website: https://www.bbc.com/news/technology-51717164
Chaturvedi A., The China way: Use of technology to combat Covid-19, Retrieved from Geospatial World website: https://www.geospatialworld.net/article/the-sino-approach-use-of-technology-to-combat-covid-19
Mijwil, M. M., and Abttan R. A., “Artificial Intelligence: A Survey on Evolution and Future Trends,” Asian Journal of Applied Sciences, vol.9, no.2, pp:87-93, April 2021 https://doi.org/10.24203/ajas.v9i2.6589
Sánchez J. M., Rodríguez J. P., and Espitia H. E., “Review of Artificial Intelligence Applied in Decision-Making Processes in Agricultural Public Policy,” Processes, vol.8, no. 1374, pp:1-23, October 2020. https://doi.org/10.3390/pr8111374
Linardatos P., Papastefanopoulos V., and Kotsiantis S., “Explainable AI: A Review of Machine Learning Interpretability Methods,” Entropy, vol.23, no.18, pp:1-45, December 2020. https://dx.doi.org/10.3390/e23010018
Ferreira J. J. and Monteiro M., “The human-AI relationship in decision-making: AI explanation to support people on justifying their decisions,” Arxiv, 2102.05460, pp:1-9, February 2021.
Soffar H., Computers in Medicine uses, advantages and disadvantages (2017), Retrieved from online-scienceswebsite: https://www.online-sciences.com/computer/computers-in-medicine-uses-advantages-and-disadvantages/
Bode C. O., “Computers in surgery,” Nigerian Journal of Surgical Research, vol.6, no.1-2, pp:1-6, 2004
Vidal F. P., Bello F., Brodlie K. W., John N. W., Gould D., Phillips R., and Avis N. J., “Principles and Applications of Computer Graphics in Medicine,” Computer Graphics forum, vol.25, no.1, pp:113-137,2006.
Xie S., Helfert M., Lugmayr A., Heimgärtner R., and Holzinger A., “Influence of Organizational Culture and Communication on the Successful Implementation of Information Technology in Hospitals,” In Proceedings of International Conference Cross-Cultural Design, pp:165-174, CCD 2013. Lecture Notes in Computer Science, vol 8024, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-39137-8_19
Sanderson M. J., Smith I., Parker I., and Bootman M. D., “Fluorescence Microscopy,” Cold Spring Harbor Laboratory Press, pp:1042-1065, November 2021. https://doi.org/10.1101/pdb.top071795
Schmidt C. W., “CT Scans: Balancing Health Risks and Medical Benefits,” Environmental Health Perspectives, vol. 120, no. 3, pp: A118-21, March 2012. https://doi.org/10.1289/ehp.120-a118
Tognarelli J M, Dawood M, Shariff M I F, Grover V P B, Crossey M M E, Cox I J, et al, “Magnetic Resonance Spectroscopy: Principles and Techniques: Lessons for Clinicians,” Journal of Clinical and Experimental Hepatology, vol.5, no.4, pp:320-328, December 2015. http://dx.doi.org/10.1016/j.jceh.2015.10.006
Shanthi D., Narsimha G., and Mohanthy R. K., “Human Intelligence vs. Artificial Intelligence: Survey,” International Journal of Electronics Communication and Computer Engineering, vol.6, no.5, pp:30-34, 2015.
Hay G. J., Klonek F. E., and Parker S. K., “Diagnosing rare diseases: A sociotechnical approach to the design of complex work systems," Applied Ergonomics, vol.86, 103095, July 2020. https://doi.org/10.1016/j.apergo.2020.103095
Nichols Z. E., and Geddes C. D., “Sample Preparation and Diagnostic Methods for a Variety of Settings: A Comprehensive Review,” Molecules, vol.26, 5666, pp:1-20, September 2021. https://doi.org/10.3390/molecules26185666
Kaur S, Singla J, Nkenyereye L, Jha S., Prashar D, Joshi G P, El-Sappagh S, et al., “Medical Diagnostic Systems Using Artificial Intelligence (AI) Algorithms: Principles and Perspectives,” IEEE Access, vo.8, pp:228049 - 228069, December 2020. https://doi.org/10.1109/ACCESS.2020.3042273
Manne R., and Kantheti S. G., “Application of Artificial Intelligence in Healthcare: Chances and Challenges,” Current Journal of Applied Science and Technology, vol.40, no.6, pp:78-89, April 2021. https://doi.org/10.9734/cjast/2021/v40i631320
Rodríguez-Rodríguez I., Rodríguez J., Shirvanizadeh N., Ortiz A., and Pardo-Quiles D., “Applications of Artificial Intelligence, Machine Learning, Big Data and the Internet of Things to the COVID-19 Pandemic: A Scientometric Review Using Text Mining,” International Journal of Environmental Research and Public Health, vol.18, 8578, pp: 1-26, August 2021. https://doi.org/10.3390/ijerph18168578
Mijwil, M. M., Al-Mistarehi, AH., and Aggarwal K., “The Effectiveness of Utilising Modern Artificial Intelligence Techniques and Initiatives to Combat COVID-19 in South Korea: A Narrative Review,” Asian Journal of Applied Sciences, vol.9, no.5, pp:343-352, November 2021. https://doi.org/10.24203/ajas.v9i5.6753
Iqbal M J, Javed Z, Sadia H, Qureshi I A, Irshad A, Ahmed R, et al., “Clinical applications of artificial intelligence and machine learning in cancer diagnosis: looking into the future,” Cancer Cell International, vol.21, Article number: 270, pp:1-11, May 2021. https://doi.org/10.1186/s12935-021-01981-1
Yassin A, Al-Mistarehi AH, El-Salem K, Urban A, Plummer C, Mohammadi S, et al., “Effect of automatic injectors on the injection latency, safety, and seizure onset zone localization of ictal single photon emission computed tomography studies in adult epilepsy monitoring unit,” Epilepsy Research, vol.169, January 2021. https://doi.org/10.1016/j.eplepsyres.2020.106522
Mirbabaie M., Stieglitz S., and Frick N. R. J., “Artificial intelligence in disease diagnostics: A critical review and classification on the current state of research guiding future direction,” Health and Technology, vol.11, pp:693–731, May 2021. https://doi.org/10.1007/s12553-021-00555-5
Yassin A., El-Salem K., Al-Mistarehi AH., “Use of Innovative SPECT Techniques in the Presurgical Evaluation of Patients with Nonlesional Extratemporal Drug-Resistant Epilepsy,” Molecular Imaging, Vol. 2021, Article ID 6614356, pp:1-9, March 2021. https://doi.org/10.1155/2021/6614356
Yassin A. M., Al-Mistarehi AH., Urban A.,and Ghearing G., “Improvement of Seizure Localization by ictal Single-Photon Emission Computed Tomography (iSPECT) Using Automatic SPECT Injectors (ASIs),” American Epilepsy Society (AES), Conference paper (abstract), November 2019. https://doi.org/10.13140/RG.2.2.19851.64804
Shademan A., Decker R. S., Opfermann J. D., et al., “Supervised autonomous robotic soft tissue surgery,” Science Translational Medicine, vol.8, no.337, p. 337ra64, May 2016. https://doi.org/10.1126/scitranslmed.aad9398
Lee DH. and Yoon S. N., “Application of Artificial Intelligence-Based Technologies in the Healthcare Industry: Opportunities and Challenges,” International Journal of Environmental Research and Public Health, vol.18, no.1, pp:1-18, January 2021. https://doi.org/10.3390/ijerph18010271
Ganasegeran K., Jamil M. F. A., Ch’ng A. S. H., Looi I., and Peariasamy K. M., “Influence of Population Density for COVID-19 Spread in Malaysia: An Ecological Study,” International Journal of Environmental Research and Public Health,vol.18, 9866, pp:1-12, September 2021, https://doi.org/10.3390/ijerph18189866.
Mijwil, M. M. and Al-Zubaidi, E. A., “Medical Image Classification for Coronavirus Disease (COVID-19) Using Convolutional Neural Networks,” Iraqi Journal of Science, vol.62, no.8, pp: 2740-2747, August 2021. https://doi.org/10.24996/ijs.2021.62.8.27.
Mohan BS., and Nambiar V., “COVID-19: An Insight into SARS-CoV-2 Pandemic Originated at Wuhan City in Hubei Province of China,” Journal of Infectious Diseases and Epidemiology, vol.6, no.4, pp:1-8, July 2020. https://doi.org/10.23937/2474-3658/1510146
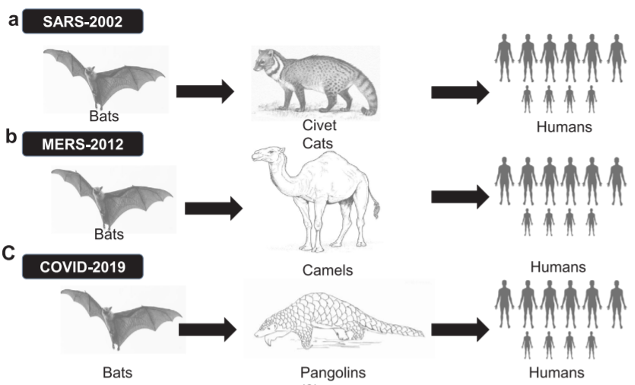
Mijwil, M. M., Alsaadi, A. S, and Aggarwal K., “Differences and Similarities Between Coronaviruses: A Comparative Review,” Asian Journal of Pharmacy, Nursing and Medical Sciences, vol.9, no.4, pp:49-61, September 2021. https://doi.org/10.24203/ajpnms.v9i4.6696
Choi J. Y., “COVID-19 in South Korea,” Postgraduate Medical Journal, vol.96, pp:399–402, May 2020, https://doi.org/10.1136/postgradmedj-2020-137738
Palaniappan A., Dave U., and Gosine B., “Comparing South Korea and Italy’s healthcare systems and initiatives to combat COVID-19,” Revista Panamericana de Salud Pública, vol.44, pp:1-5, April 2020. https://doi.org/10.26633/RPSP.2020.53
Bragazzi N. L., Dai H., Damiani G., Behzadifar M., Martini M., and Wu J., “How Big Data and Artificial Intelligence Can Help Better Manage the COVID-19 Pandemic,” International Journal of Environmental Research and Public Health, vol.17, 3176, pp:1-8, May 2020. https://doi.org/10.3390/ijerph17093176
Anhlan D., Grundmann N., Makalowski W., Ludwig S., and Scholtissek C., “Origin of the 1918 pandemic H1N1 influenza A virus as studied by codon usage patterns and phylogenetic analysis,” RNA (New York, N.Y.), vol.17, pp:64–73, January 2011. https://doi.org/10.1261/rna.2395211
Violato C., Violato E. M., and Violato E. M., “Impact of the stringency of lockdown measures on covid-19: A theoretical model of a pandemic,” PLOS ONE, vol.16, no.10, pp:1-14, October 2021. https://doi.org/10.1371/journal.pone.0258205
Samrah S M, Al-Mistarehi AH W, Ibnian A M, Raffee L A, Momany S M, Al-Ali M, et al., COVID-19 outbreak in Jordan: Epidemiological features, clinical characteristics, and laboratory findings, Annals of Medicine and Surgery, vol.57, pp: 103-108, September 2020. https://doi.org/10.1016/j.amsu.2020.07.020
Ramadan M, Hasan Z, Saleh T, Jaradat M, Al-hazaimeh M, Hani O B, et al., “Beyond knowledge: Evaluating the practices and precautionary measures towards COVID-19 amongst medical doctors in Jordan,” International Journal of Clinical Practice, vol.75, pp: e14122, March 2021. https://doi.org/10.1111/ijcp.14122
Khassawneh A. H., Alrabadi N., Al-Mistarehi AH., Obeidat N., and Kheirallah K. A., “The role of non-state actors in combating COVID-19 spread in Northern Jordan,” Annals of Medicine and Surgery, vol.60, pp:484-486, December 2020. https://doi.org/10.1016/j.amsu.2020.11.005
Wildman J. M., Morris S., Pollard T., Gibson K., and Moffatt S., ““I wouldn't survive it, as simple as that”: Syndemic vulnerability among people living with chronic non-communicable disease during the COVID-19 pandemic,” SSM - Qualitative Research in Health, vol.2, pp:1-8, December 2022. https://doi.org/10.1016/j.ssmqr.2021.100032
Samrah S M, Al-Mistarehi AH, Aleshawi A J, Khasawneh A G, Momany S M, Momany B S et al., “Depression and Coping Among COVID-19-Infected Individuals After 10 Days of Mandatory in-Hospital Quarantine, Irbid, Jordan,” Psychology Research and Behavior Management, vol.13, pp: 823—830, October 2020. https://doi.org/10.2147/PRBM.S267459
Al-Shatanawi T N, Sakka S A, Kheirallah K A, Al-Mistarehi AH, Al-Tamimi S, Alrabadi N, et al., “Self-Reported Obsession Toward COVID-19 Preventive Measures Among Undergraduate Medical Students During the Early Phase of Pandemic in Jordan,” Frontiers in Public Health, vol.9, pp:1-13, November 2021. https://doi.org/10.3389/fpubh.2021.719668
Kheirallah K., Bloukh S., Khasawneh W., Alsulaiman J, Khassawneh A, Al-Mistarehi AH, et al., “Medical students’ relative immunity, or lack thereof, against COVID-19 emotional distress and psychological challenges; a descriptive study from Jordan,” f1000research, pp:1-18, November 2021. https://doi.org/10.12688/f1000research.52051.2
Altig D., Baker S., Barrero J. M., “Economic uncertainty before and during the COVID-19 pandemic,” Journal of Public Economics, vol.191, pp:1-13, November 2020. https://doi.org/10.1016/j.jpubeco.2020.104274
Rossi R, Socci V, Talevi D, Mensi S, NioluC, Pacitti F, et al. “COVID-19 Pandemic and Lockdown Measures Impact on Mental Health Among the General Population in Italy,” Frontiers in Psychology, vol.11, pp:1-6, August 2020. https://doi.org/10.3389/fpsyt.2020.00790
Emanuel E J, Persad G, Upshur R, Thome B, Parker M, Glickman A, et al. “Fair Allocation of Scarce Medical Resources in the Time of Covid-19,” The New England Journal of Medicine, vol.382, pp:2049-2055, May 2020. https://doi.org/10.1056/NEJMsb2005114
Yassin A, Ghzawi A, Al-Mistarehi AH, El-Salem K, Benmelouka A Y, Sherif A M, et al. “Mortality rate and biomarker expression within COVID-19 patients who develop acute ischemic stroke: a systematic review and meta-analysis,” Future Science OA, vol. 7, no. 7, pp:1-14, August 2021. https://doi.org/10.2144/fsoa-2021-0036
Özdemir Ö., “Coronavirus Disease 2019 (COVID-19): Diagnosis and Management,” Erciyes Medical Journal, vol.42, no.3, pp: 242–247, April 2020. https://doi.org/10.14744/etd.2020.99836
Tsao S., Chen H., Tisseverasinghe T., Yang Y., Li L., and Butt Z. A., “What social media told us in the time of COVID-19: a scoping review,” The Lancet Digital Health, vol.3, no.3,pp: E175-E194, March 2021. https://doi.org/10.1016/S2589-7500(20)30315-0
Vallamkondu J, John A, Wani W Y, Ramadevi S P, Jella K K, Reddy P H, et al “SARS-CoV-2 pathophysiology and assessment of coronaviruses in CNS diseases with a focus on therapeutic targets,” BBA - Molecular Basis of Disease, pp:1-13, June 2020. https://doi.org/10.1016/j.bbadis.2020.165889
Kheirallah K A, Al-Mistarehi AH, Alsawalha L, Hijazeen Z, Mahrous H, Sheikali S, et al. “Prioritizing zoonotic diseases utilizing the One Health approach: Jordan's experience,” One Health, pp:1-10, vol.13, pp:1-10, December 2021. https://doi.org/10.1016/j.onehlt.2021.100262
Wang L. F. and Crameri G., “Emerging zoonotic viral diseases,” Revue scientifique et technique, vol.33, no. 2, pp:569-581, August 2014. http://dx.doi.org/10.20506/rst.33.2.2311
Singanayagam A, Hakki S, Dunning J, Madon K J, Crone M A, Koycheva A, et al., “Community transmission and viral load kinetics of the SARS-CoV-2 delta (B.1.617.2) variant in vaccinated and unvaccinated individuals in the UK: a prospective, longitudinal, cohort study,” Lancet Infect Diseases, pp:1-13, October 2021. https://doi.org/10.1016/S1473-3099(21)00648-4
Bar-On Y. M., Flamholz A., Phillips R., and MiloI R., “SARS-CoV-2 (COVID-19) by the numbers,” eLife, vol.9, pp:1-15, April 2020. https://doi.org/10.7554/eLife.57309
Samrah S M, Al-Mistarehi AH, Kewan T, Al-Khatib S M, Ibnian A M, Samrah R S, Khassawneh B Y. “Viral Clearance Course of COVID-19 Outbreaks,” Journal of Multidisciplinary Healthcare, vol.14, pp: 555–565, March 2021. https://doi.org/10.2147/JMDH.S302891
Viner R. M., Ward J. L., Hudson, L. D., Ashe M., Patel S. V., Hargreaves D., and Whittaker E., “Systematic review of reviews of symptoms and signs of COVID-19 in children and adolescents,” Archives of Disease in Childhood, vol.106, pp:802–807, December 2020. https://doi.org/10.1136/archdischild-2020-320972
Hu B., Guo H., Zhou P., and Shi Z., “Characteristics of SARS-CoV-2 and COVID-19,” Nature reviews Microbiology, vol.19, pp:141–154, October 2020. https://doi.org/10.1038/s41579-020-00459-7
Samrah S M, Al-Mistarehi AH W, Ibnian A M, Raffee L A, Momany S M, Al-Ali M, et al. “COVID-19 outbreak in Jordan: Epidemiological features, clinical characteristics, and laboratory findings,” Annals of Medicine and Surgery, vol.57, pp:103-108, September 2020. https://doi.org/10.1016/j.amsu.2020.07.020
Wang D, Hu B, Chang Hu C, Zhu F, Liu X, Zhang J, et al., Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China, JAMA, vol.323, no.11, pp:1061-1069, February 2020. https://doi.org/10.1001/jama.2020.1585
Shen C., Yue X., Wang J., Shi C., and Li W., “Nocturnal oxygen therapy as an option for early COVID-19,” International Journal of Infectious Diseases, vol. 98, pp:167-179, September 2020. https://doi.org/10.1016/j.ijid.2020.06.080
Mellado‑Artigas R, Ferreyro B L, Angriman F, María Hernández‑Sanz M, Arruti B, Torres A, et al. “High‑fow nasal oxygen in patients with COVID‑19‑associated acute respiratory failure,” Critical Care, vol.25, Article number: 58, February 2021. https://doi.org/10.1186/s13054-021-03469-w
Shen C., Yue X., Wanga J., Shi C., and Li W., “Nocturnal oxygen therapy as an option for early COVID-19,” International Journal of Infectious Diseases, vol.98, pp:176-179, June 2020. https://doi.org/10.1016/j.ijid.2020.06.080
Ferdinand P. and Roffe C., “Hypoxia after stroke: a review of experimental and clinical evidence,” Experimental & Translational Stroke Medicine, vol. 8, Article number: 9, pp:1-8, December 2016. https://doi.org/10.1186/s13231-016-0023-0
Sunde G A, Sandberg M, Lyon R, Fredriksen K, Burns B, Hufthammer K O, et al ., “Hypoxia and hypotension in patients intubated by physician staffed helicopter emergency medical services - a prospective observational multi-centre study,” BMC Emergency Medicine, vol. 17, Article number: 22, July 2017. https://doi.org/10.1186/s12873-017-0134-5
Coccia C. B. I., Palkowski G. H., Schweitzer B., Motsoh T., and Ntusi N. A. B., “Dyspnoea: Pathophysiology and a clinical approach,” South African Medical Journal, vol.106, no.1, pp:32-36, January 2016. https://doi.org/10.7196/SAMJ.2016.v106i1.10324
Scott J. B., and Kaur R., “Monitoring Breathing Frequency, Pattern, and Effort, Respiratory Care,” vol.65, no.6, pp: 793-806, June 2020. https://doi.org/10.4187/respcare.07439
Guo D., Pan S., Wang M., and Guo Y., “Hyperbaric oxygen therapy may be effective to improve hypoxemia in patients with severe COVID-2019 pneumonia: two case reports,” Undersea & Hyperbaric Medical Society, 2020 Second-Quarter; vol.7, no.2, pp:181-187. https://doi.org/10.22462/04.06.2020.2
Bracegirdle L., Beecham R., Jackson A., Dushianthan A., and Cumpstey A. (2021), Total Arterial Oxygen Content in Patients Admitted to Intensive Care With Hypoxaemic Respiratory Failure Due to Covid-19, Retrieved from Waitmeeting website: https://www.waitmeeting.org/posters_2021/Luke_Bracegirdle.pdf
Liu Y., Wen B., Zhang F., and Pan X., “Effects of blood oxygen saturation on pulmonary artery remodeling in an in vitro perfusion circuit model,” Journal of Thoracic Disease, vol.13, no.4, pp:2169-2176, April 2021. http://dx.doi.org/10.21037/jtd-20-2124
Bluemke E., Stride E., and Bulte D. P., “A General Model to Calculate the Spin–Lattice Relaxation Rate (R1) of Blood, Accounting for Hematocrit, Oxygen Saturation, Oxygen Partial Pressure, and Magnetic Field Strength Under Hyperoxic Conditions,” Journal of Magnetic Resonance Imaging, pp:1-12, October 2021. https://doi.org/10.1002/jmri.27938
Sharma S. and Rawat D., Partial Pressure of Oxygen (PO2) (2018), Retrieved from ResearchGate website: https://www.researchgate.net/publication/324683692_Partial_Pressure_Of_Oxygen_PO2
Golub A. S., Dodhy S. C., and Pittman R. N., “Oxygen dependence of respiration in rat spin trapezius muscle contracting at 0.5–8 twitches per second,” Journal of Applied Physiology, vol.125, no.1, pp:124-133, July 2018. https://doi.org/10.1152/japplphysiol.01136.2016
Papazian L, Aubron C, Brochard L, Chiche JD, Combes A, Dreyfuss D, et al. “Formal guidelines: management of acute respiratory distress syndrome,” Annals of Intensive Care, vol. 9, Article number: 69, pp:1-18, June 2019. https://doi.org/10.1186/s13613-019-0540-9
Saguil A., and Fargo M. V., “Acute Respiratory Distress Syndrome: Diagnosis and Management,” American Family Physician, vol.101, no.12, pp:730-738, Jun 2020.
Wu Z. and McGoogan J. M., “Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention,” JAMA Network, vol.323, no.13, pp:1239-1242, February 2020. https://doi.org/110.1001/jama.2020.2648
Stokes E. K., Zambrano L. D., Anderson K. N., Marder E. P., Raz K. M., Felix S. E. B., Tie Y., and Fullerton K. E., “Coronavirus Disease 2019 Case Surveillance — United States, January 22–May 30, 2020,” Morbidity and Mortality Weekly Report, vol.69, no.24, pp:759-765, June 2020.
Li J, Huang D Q, Zou B Z, Yang H, Hui W Z, Rui F, et al., “Epidemiology of COVID-19: A systematic review and meta-analysis of clinical characteristics, risk factors, and outcomes,” Journal of Medical Virology, vol.93, no.3, pp:1449-1458, August 2020. https://doi.org/10.1002/jmv.26424
Hasan A, Paray B A, Hussain A, Qadire F A, Attarf F, Aziz F M, et al., “A review on the cleavage priming of the spike protein on coronavirus by angiotensin-converting enzyme-2 and furin,” Journal of Biomolecular Structure and Dynamics, pp:1-9, April 2020. https://doi.org/10.1080/07391102.2020.1754293
Murdaca G., Gioacchino M., Greco M., Borro M., Paladin F., Petrarca C., and Gangemi S., “Basophils and Mast Cells in COVID-19 Pathogenesis,” Cells, vol.10, 2754, pp:1-13, October 2021. https://doi.org/10.3390/cells10102754
Ghaebi M., Osali A., Valizadeh H., Roshangar L., and Ahmadi M., “Vaccine development and therapeutic design for 2019-nCoV/SARS-CoV-2: Challenges and chances,” Journal of Cellular Physiology, vol.235, pp:9098–9109, June 2020. https://doi.org/10.1002/jcp.29771
Al-Mistarehi AH, Kheirallah K A, Yassin A, Alomari S, Aledrisi M K, Ata E M B, et al. “Determinants of the willingness of the general population to get vaccinated against COVID-19 in a developing country,” Clinical and Experimental Vaccine Research, vol.10, no.2, pp:171–182, May 2021. https://doi.org/10.7774/cevr.2021.10.2.171
Chaudhary N., Weissman D., and Whitehead K. A., “mRNA vaccines for infectious diseases: principles, delivery and clinical translation,” Nature Reviews Drug Discovery, vol.20, pp:817–838, August 2021. https://doi.org/10.1038/s41573-021-00283-5
Chavda V. P., Pandya R., and Apostolopoulos V., “DNA vaccines for SARS-CoV-2: toward third generation vaccination era,” Expert Review of Vaccines, pp:1-13, October 2021. https://doi.org/10.1080/14760584.2021.1987223
Condit R C, Kim D, Robertson J S, Excler JL, Gurwith M, Monath T P C, et al. “The Brighton Collaboration standardized template for collection of key information for benefit-risk assessment of viral vector vaccines,” Vaccine, vol. 38, no. 49, pp: 7708-7715, November 2020. https://doi.org/10.1016/j.vaccine.2020.08.009
Wang N., Shang J., Jiang S., and Du L., “Subunit Vaccines Against Emerging Pathogenic Human Coronaviruses,” Frontiers in Microbiology, vol.11, Article 298, pp:1-19, February 2020. https://doi.org/10.3389/fmicb.2020.00298
Quan F., Basak S., Chu K., Kim S. S., and Kang S., “Progress in the development of virus-like particle vaccines against respiratory viruses,” Expert Review of Vaccines, vol.19, no.1, pp:11-24, January 2020. https://doi.org/10.1080/14760584.2020.1711053
Liu W, Nachbagauer R, Stadlbauer D, Strohmeier S, Solórzano A, Berlanda-Scorza F, et al. “Chimeric Hemagglutinin-Based Live-Attenuated Vaccines Confer Durable Protective Immunity against Influenza A Viruses in a Preclinical Ferret Model,” Vaccines, vol.9, no.40, pp:1-18, January 2021. https://doi.org/10.3390/vaccines901004
Palacios R, Patiño E G, Piorelli R O, Conde M T R P, Batista A P, Zeng G, et al., “Double-Blind, Randomized, PlaceboControlled Phase III Clinical Trial to Evaluate the Efficacy and Safety of treating Healthcare Professionals with the Adsorbed COVID-19 (Inactivated) Vaccine Manufactured by Sinovac – PROFISCOV: A structured summary of a study protocol for a randomised controlled trial,” Trials, vol.21, Article number 853, pp:1-3, October 2020. https://doi.org/10.1186/s13063-020-04775-4
González-Rivero M, Beijbom O, Rodriguez-Ramirez A, Bryant D E P, and Ganase A, “Monitoring of Coral Reefs Using Artificial Intelligence: A Feasible and Cost-Effective Approach,” Remote Sensing, vol.12, no.489, pp:1-22, February 2020. https://doi.org/10.3390/rs12030489
Mijwil M. M. and Abttan R. A., “Applying Genetic Algorithm to Optimization Second-Order Bandpass MGMFB Filter,” Pertanika Journal of Science and Technology, vol.28, no.4, pp. 1413–1425, October 2020. https://doi.org/10.47836/pjst.28.4.15.
Jiménez-Luna J., Grisoni F., and Schneider G., “Drug discovery with explainable artificial intelligence,” Nature Machine Intelligence, vol.2, pp:573–584, October 2020. https://doi.org/10.1038/s42256-020-00236-4.
Mijwil, M. M., “Malware Detection in Android OS Using Machine Learning Techniques,” Data Science and Applications, vol.3, no.2, pp:5-9, December 2020.
Ahmed S. R., Abbood Z. A., Farhan H. M., Yasen B. T., Ahmed M. R.,and Duru A. D., "Speaker Identification Model Based on Deep Neural Networks". Iraqi Journal For Computer Science and Mathematics, vol.3 , no.1, pp: 108-114, January 2022.
Shah D., Patel S., and Bharti S. K., “Heart Disease Prediction using Machine Learning Techniques,” SN Computer Science, vol. 1, Article number 345, pp:1-6, October 2020. https://doi.org/10.1007/s42979-020-00365-y
Yang Z, Zeng Z, Wang K, Won S, Liang W, Zanin M, et al. “Modified SEIR and AI prediction of the epidemics trend of COVID-19 in China under public health interventions,” Journal of Thoracic Disease, vol.12, no.3, pp: 165-174, March 2020. http://dx.doi.org/10.21037/jtd.2020.02.64
Qin L., Sun Q., Wang Y., Wu K., Chen M., Shia B., and Wu S, “Prediction of Number of Cases of 2019 Novel Coronavirus (COVID-19) Using Social Media Search Index,” International Journal of Environmental Research and Public Health, vol.12, 2365, pp:1-14, March 2020. https://doi.org/10.3390/ijerph17072365
Ko G. S., and Yoon T., “Short-Term Prediction Methodology of COVID-19 Infection in South Korea,” COVID, vol.1, no.1, pp:416-422, September 2021. https://doi.org/10.3390/covid1010035
Li S., Wang Y., Xue J., Zhao N., and Zhu T., “The Impact of COVID-19 Epidemic Declaration on Psychological Consequences: A Study on Active Weibo Users,” International Journal of Environmental Research and Public Health, vol. 17, 2032, pp:1-9, March 2020. https://doi.org/10.3390/ijerph17062032
Irvin J, Rajpurkar P, Ko M, Yu Y, Ciurea-Ilcus S, Chute C, et al. “CheXpert: A Large Chest Radiograph Dataset with Uncertainty Labels and Expert Comparison,” Proceedings of the AAAI Conference on Artificial Intelligence 33, pp:590-597, July 2019. https://doi.org/10.1609/aaai.v33i01.3301590
Minaee S., Kafieh R., Sonka M., Yazdani S., and Soufi G. J., “Deep-COVID: Predicting COVID-19 from chest X-ray images using deep transfer learning,” Medical Image Analysis, vol. 65, no.101794, pp:1-9, October 2020. https://doi.org/10.1016/j.media.2020.101794
Meng Z., Wang M., Song H., Guo S, Zhou Y, Li W, et al. “Development and utilization of an intelligent application for aiding COVID-19 diagnosis,” MedRxiv, pp:1-21, March 2020. https://doi.org/10.1101/2020.03.18.20035816
Gong J, Ou J, Qiu X, Jie Y, Chen Y, Yuan L, et al. “A Tool to Early Predict Severe Corona Virus Disease 2019 (COVID-19): A Multicenter Study using the Risk Nomogram in Wuhan and Guangdong, China,” Clinical Infectious Diseases, vol.71, no.15, pp: 833-840, August 2020. https://doi.org/10.1093/cid/ciaa443
Sun L, Song F, Shi N, Liu F, Li S, Li P, et al., “Combination of four clinical indicators predicts the severe/critical symptom of patients infected COVID-19,” Journal of Clinical Virology, vol.128, 104431, pp:1-6, July 2020. https://doi.org/10.1016/j.jcv.2020.104431
Yan L, Zhang H, Goncalves J, Xiao Y, Wang M, Guo Y, et al. “An interpretable mortality prediction model for COVID-19 patients,” Nature Machine Intelligence, vol. 2, pp: 283–288, May 2020. https://doi.org/10.1038/s42256-020-0180-7
Brinati D., Campagner A., Ferrari D., Locatelli M., Banf G., and Cabitza F., “Detection of COVID-19 Infection from Routine Blood Exams with Machine Learning: A Feasibility Study,” Journal of Medical Systems, vol.44, 135, pp:1-12, July 2020. https://doi.org/10.1007/s10916-020-01597-4
Yu H., Shao J., Guo Y., Xiang Y., Sun C., and Yuan Y., “Data-driven discovery of a clinical route for severity detection of COVID-19 pediatric cases,” Medrxiv, pp:1-6, March 2020. https://doi.org/10.1101/2020.03.09.20032219
Yadaw A. S., Li Y., , Bose S., Iyengar R., Bunyavanich S., and Pandey G., “Clinical features of COVID-19 mortality: development and validation of a clinical prediction model,” Lancet Digital Health, vol.2, no.10, pp:E516-E525, October 2020. https://doi.org/10.1016/S2589-7500(20)30217-X
Berenguer J, Borobia A M, Ryan P, Rodríguez-Baño J, Bellón J M, Jarrín I, et al. “Development and validation of a prediction model for 30-day mortality in hospitalised patients with COVID-19: the COVID-19 SEIMC score,” Thorax, vol.76, no.9, pp:920–929, August 2021. https://doi.org/10.1136/thoraxjnl-2020-216001
Ikemura K., Bellin E., Yagi Y., Billett H, Saada M, Simone K, et al., “Using Automated Machine Learning to Predict the Mortality of Patients With COVID-19: Prediction Model Development Study,” Journal of Medical Internet Research, vol.23, no.2, pp:1-15, February 2021. https://doi.org/10.2196/23458
Statsenko Y., Al Zahmi F., Habuza T., Gorkom K. N., and Zaki N., “Prediction of COVID-19 severity using laboratory findings on admission: informative values, thresholds, ML model performance,” BMJ Open, vol.11, no.2, pp:1-13, February 2021. https://doi.org/10.1136/bmjopen-2020-044500
Xumao Z., Xiang L., and Xinhai L., “Tracking the spread of novel coronavirus (2019-nCoV) based on big data,” MedRxiv, pp:1-9, February 2020. https://doi.org/10.1101/2020.02.07.20021196
Githinji G., Laurent Z. R., Mohammed K. S., Omuoyo D. O., et al., “Tracking the introduction and spread of SARS-CoV-2 in coastal Kenya,” Nature Communications, vol.12, no.4809, pp:1-10, August 2021. https://doi.org/10.1038/s41467-021-25137-x
Benreguia B., Moumen H., and Merzoug M. A., “Tracking COVID-19 by Tracking Infectious Trajectories,” IEEE Access, vol.8, pp:145242 – 145255, August 2020. https://doi.org/10.1109/ACCESS.2020.3015002
Bowling M., Fürnkranz J., Graepel T., and Musick R., “Machine learning and games,” Machine Learning, vol. 63, pp:211–215, May 2006. https://doi.org/10.1007/s10994-006-8919-x
Schwartz W. B., “Medicine and the Computer: The Promise and Problems of Change,” In Use and impact of computers in clinical medicine, pp. 321-335. Springer, New York, NY, 1970. https://doi.org/10.1007/978-1-4613-8674-2_20
Pesapane F., Codari M., and Sardanelli F., “Artificial intelligence in medical imaging: threat or opportunity? Radiologists again at the forefront of innovation in medicine,” European Radiology Experimental, vol. 2, Article number: 35, pp:1-10, October 2018. https://doi.org/10.1186/s41747-018-0061-6
Aggarwal K., Mijwil M. M., Al-Mistarehi AH., Alomari S., Gök M., Alaabdin A. M. Z., and Abdulrhman S. H., “Has the Future Started? The Current Growth of Artificial Intelligence, Machine Learning, and Deep Learning,” Iraqi Journal for Computer Science and Mathematics, vol.3, no.1, pp:115-123, January 2022.
Farhan B. I. and Jasim A. D. “A Survey of Intrusion Detection Using Deep Learning in Internet of Things”, Iraqi Journal For Computer Science and Mathematics, vol. 3, no. 1, pp. 83-93, January 2022.
Rammo F. M. and Al-Hamdani M. N., “Detecting The Speaker Language Using CNN Deep Learning Algorithm”, Iraqi Journal For Computer Science and Mathematics, vol. 3, no. 1, pp. 43-52, January 2022.
Mijwil, M. M., Salem I. E, and Abttan R. A. “Utilisation of Machine Learning Techniques in Testing and Training of Different Medical Datasets,” Asian Journal of Computer and Information Systems, vol.9, no.5, pp:29-34, November 2021, https://doi.org/10.24203/ajcis.v9i4.6765
Ahmed S., Abbood Z. A., Farhan H. M., Yasen B. T., Ahmed M. R., and Duru A. D., “Speaker Identification Model Based on Deep Neural Networks”, Iraqi Journal For Computer Science and Mathematics, vol. 3, no. 1, pp. 108-114, January2022.
Adedigba A. P., Adeshina S. A., Aina O. E., and Aibinu A. M., “Optimal hyperparameter selection of deep learning models for COVID-19 chest X-ray classification,” Intelligence-Based Medicine, vol.5, 100034, pp:1-5, 2021. https://doi.org/10.1016/j.ibmed.2021.100034
Rahimzadeh M. and Attar A., “A modified deep convolutional neural network for detecting COVID-19 and pneumonia from chest X-ray images based on the concatenation of Xception and ResNet50V2,” Informatics in Medicine Unlocked, vol.19, pp:1-9, May 2020. https://doi.org/10.1016/j.imu.2020.100360
Narin A., Kaya C., and Pamuk Z., “Automatic Detection of Coronavirus Disease (COVID-19) Using X-ray Images and Deep Convolutional Neural Networks,” Pattern Analysis and Applications, vol.24, pp:1207–1220, May 2020. https://doi.org/10.1007/s10044-021-00984-y
Apostolopoulos I. D., Aznaouridis S. I., and Tzani M. A., “Extracting Possibly Representative COVID‑19 Biomarkers from X‑ray Images with Deep Learning Approach and Image Data Related to Pulmonary Diseases,” Journal of Medical and Biological Engineering, vol. 40, pp:462–469, May 2020. https://doi.org/10.1007/s40846-020-00529-4
Mahmud T., Rahman A., and Fattah S. A., “CovXNet: A multi-dilation convolutional neural network for automatic COVID-19 and other pneumonia detection from chest X-ray images with transferable multi-receptive feature optimization,” Computers in Biology and Medicine, vol.122, pp:1-10, July 2020. https://doi.org/10.1016/j.compbiomed.2020.103869
Sathitratanacheewin S., Sunanta P., and Pongpirul K., “Deep learning for automated classification of tuberculosis-related chest X-Ray: dataset distribution shift limits diagnostic performance generalizability,” Heliyon, vol.6, no.8, pp:1-4, August 2020. https://doi.org/10.1016/j.heliyon.2020.e04614
Duran-Lopez L., Dominguez-Morales J. P., Corral-Jaime J., Vicente-Diaz S., and Linares-Barranco A., “COVID-XNet: A Custom Deep Learning System to Diagnose and Locate COVID-19 in Chest X-ray Images,” Applied Sciences, vol.10, no.16, pp:1-12, August 2020. https://doi.org/10.3390/app10165683
Sekeroglu B. and Ozsahin I., “Detection of COVID-19 from Chest X-Ray Images Using Convolutional Neural Networks,” SLAS Technology, vol.25, no.6, pp:553–565, September 2020. https://doi.org/10.1177/2472630320958376
Abbas A., Abdelsamea M. M., and Gaber M. M., “Classification of COVID-19 in chest X-ray images using DeTraC deep convolutional neural network,” Applied Intelligence, vol.51, pp:854–864, September 2020. https://doi.org/10.1007/s10489-020-01829-7
Maguolo G. and Nanni L., “A Critic Evaluation of Methods for COVID-19 Automatic Detection from X-Ray Images,” Arxiv, pp:1-10, September 2020. https://arxiv.org/abs/2004.12823
Wang L., Lin Z. Q., and Wong A., “COVID‑Net: a tailored deep convolutional neural network design for detection of COVID‑19 cases from chest X‑ray images,” Scientifc Reports, vol.10, Article number: 19549, pp:1-12, November 2020. https://doi.org/10.1038/s41598-020-76550-z
Khan A. I., Shah J. L., and Bhat M. M., “CoroNet: A deep neural network for detection and diagnosis of COVID-19 from chest x-ray images,” Computer Methods and Programs in Biomedicine, vol.196, pp:1-9, November 2020. https://doi.org/10.1016/j.cmpb.2020.105581
Ibrahim A. U., Ozsoz M., Serte S., Al‑Turjman F., and Yakoi P. S., “Pneumonia Classifcation Using Deep Learning from Chest X‑ray Images During COVID‑19,” Cognitive Computation, pp:1-13, January 2021. https://doi.org/10.1007/s12559-020-09787-5
Alam N. A., Ahsan M., Based A., Haider J., and Kowalski M., “COVID-19 Detection from Chest X-ray Images Using Feature Fusion and Deep Learning,” Sensors, vol.21, no.4, pp: 1-26, February 2021. https://doi.org/10.3390/s21041480
Polat Ç., Karaman O., Karaman C., Korkmaz G., Balcı M. C., and Kelek S. E., “COVID-19 diagnosis from chest X-ray images using transfer learning: Enhanced performance by debiasing dataloader,” Journal of X-Ray Science and Technology, vol.29, no.1, pp:19-36, February 2021. https://doi.org/10.3233/XST-200757
Shelke A., Inamdar M., Shah V., Tiwari A., Hussain A., Chafekar T., and Mehendale N., “Chest X‑ray Classifcation Using Deep Learning for Automated COVID‑19 Screening,” SN Computer Science, vol.2, Article number: 300, pp:1-9, May 2021. https://doi.org/10.1007/s42979-021-00695-5
Cortés E. and Sánchez S., “Deep Learning Transfer with AlexNet for chest X-ray COVID-19 recognition,” IEEE Latin America Transactions, vol.19, No.6, pp:944-951, June 2021.
Mijwil, M. M., “Implementation of Machine Learning Techniques for the Classification of Lung X-Ray Images Used to Detect COVID-19 in Humans,” Iraqi Journal of Science, vol.62, no.6., pp: 2099-2109, July 2021. https://doi.org/10.24996/ijs.2021.62.6.35.
Khasawneh N., Fraiwan M., Fraiwan L., Khassawneh B., and Ibnian A., “Detection of COVID-19 from Chest X-ray Images Using Deep Convolutional Neural Networks,” Sensors, vol.21, no.17, pp:1-15, September 2021. https://doi.org/10.3390/s21175940
Badawi A. and Elgazzar K., “Detecting Coronavirus from Chest X-rays Using Transfer Learning,” COVID, vol.1, no.1, pp:403-415, September 2021. https://doi.org/10.3390/covid1010034
Downloads
Published
Issue
Section
License
Copyright (c) 2021 Maad Mijwil, Abdel-Hameed Al-Mistarehi, Dhamyaa Salim Mutar

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Start from 2019 issues, authors who publish with JURNAL MOBILE AND FORENSICS agree to the following terms:
- Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License (CC BY-SA 4.0) that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.









 Mobile and Forensics (MF)
Mobile and Forensics (MF)