Buletin Ilmiah Sarjana Teknik Elektro ISSN: 2685-9572
Bibliometric Analysis of Explainable AI in Advance Care Planning: Insights, Collaborative Trends, and Future Prospects
Irianna Futri 1, Elvaro Islami Muryadi 2,3, Dimas Chaerul Ekty Saputra 4,5
1 Department of International Technology and Innovation Management, International College, Khon Kaen University,
Khon Kaen 40002, Thailand
2 Department of Community, Occupational, and Family Medicine, Faculty of Medicine, Khon Kaen University, Khon
Kaen 40002, Thailand
3 Department of Public Health, Faculty of Health Sciences, Adiwangsa Jambi University, Jambi 36138, Indonesia
4 Department of Informatics, School of Computing, Telkom University, Surabaya 60231, Indonesia
5 Department of Computer Science, College of Computing, Khon Kaen University, Khon Kaen 40002, Thailand
ARTICLE INFORMATION |
| ABSTRACT |
Article History: Received 28 September 2024 Revised 04 December 2024 Published 12 December 2024 |
| 
The increasing complexity of healthcare systems has led to a growing need for Advance Care Planning (ACP) to ensure personalized care for patients. Explainable Artificial Intelligence (XAI) has emerged as a promising solution to enhance ACP by providing transparent and interpretable decision-making processes. However, the current landscape of XAI in ACP remains unclear, necessitating a comprehensive bibliometric analysis. This study employed a systematic review of existing literature on XAI in ACP, using a bibliometric approach to analyze publication trends, collaboration patterns, and research themes. One hundred sixty articles were selected from prominent databases, and their metadata were extracted and analyzed using Biblioshiny, the analysis revealed a significant growth in ACP XAI-related publications, focusing on deep learning and natural language processing techniques. The top contributing authors and institutions were identified, and their collaborative networks were visualized. The results also highlighted the prominent themes of patient-centered care, decision support systems, and healthcare analytics. The study's findings have implications for developing more effective XAI-based ACP systems. This bibliometric analysis provides valuable insights into the current state of XAI in ACP, highlighting the need for further research and collaboration to address the complex challenges in healthcare. The study's outcomes can inform policymakers, researchers, and practitioners in developing more effective ACP systems that leverage the potential of XAI. |
Keywords: Explainable AI; Advance Care Planning; Bibliometric Analysis; Healthcare Analytics; Decision Support Systems |
Corresponding Author: Dimas Chaerul Ekty Saputra, Telkom University, Surabaya 60231, Indonesia. Email: dimaschaerulekty@telkomuniversity.ac.id |
This work is licensed under a Creative Commons Attribution-Share Alike 4.0 
|
Document Citation: I. Futri, E. I. Muryadi, and D. C. E. Saputra, “Bibliometric Analysis of Explainable AI in Advance Care Planning: Insights, Collaborative Trends, and Future Prospects,” Buletin Ilmiah Sarjana Teknik Elektro, vol. 6, no. 4, pp. 334-356, 2024, DOI: 10.12928/biste.v6i4.11641. |
INTRODUCTION
Globally, the phenomenon of an aging population is getting more noticeable and seriously affecting public welfare. Data from the World Health Organisation (WHO) show that 1.4 billion individuals 65 years of age and over would be expected to rise to 2.1 billion by 2025 [1]. Although higher-income nations show this demographic change most clearly, other nations like Asia and Europe also see similar patterns with increasing numbers of elderly individuals [2][3]. For healthcare systems, this demographic shift poses significant difficulties, especially in terms of managing chronic conditions that disproportionately impact elderly individuals [4]. Diseases including cancer, heart disease, and dementia call for not only excellent medical therapy but also thorough planning to guarantee that patients' values and preferences are honoured all through their treatment paths.
The prevalence of chronic diseases is expected to rise as the population ages, increasing the demand for healthcare services [5][6]. Particularly about life-limiting diseases, elderly individuals frequently have complicated medical problems that call for considerable thought on their treatment preferences [7]. However, many individuals lack knowledge of advance care planning (ACP), so they are not ready to discuss their end-of-life treatment choices. As a result, doctors often make judgments without enough awareness of the values and preferences of patients[8][9]. This mismatch emphasizes the need for improved communication since it can lead to treatment that does not appeal to the individual's preferences.
Advance care planning (ACP) is a proactive process that enables individuals to articulate their preferences regarding future medical care, particularly in the context of serious illnesses [10][11].The primary aims of Advance care planning (ACP) include ensuring that individual values and wishes are honored and facilitating informed decision-making among healthcare providers and family members [12][13]. The early start of these processes helps individuals match their healthcare with their values and reduces the possibility of unnecessary treatments [14]. Furthermore, Advance care planning (ACP) helps reduce family members' emotional burden during crises[15]. Establishing a hospital environment that values individual-centered care, especially for the aged, depends on raising knowledge of advance care planning and understanding it.
Technological advances in healthcare have brought about significant changes in how healthcare is delivered, including in the context of advance care planning (ACP). Information and communication technologies allow patients and healthcare providers to interact more efficiently and effectively, facilitating discussions about care preferences [16][17]. In addition, digital apps and platforms can help individuals develop their care plans, store necessary documentation, and access information about available care options [18][19]. Artificial intelligence (AI) is also beginning to play a role in advance care planning (ACP), with tools that can analyze data and provide recommendations based on patient preferences and their health conditions [20]. The integration of these technologies makes the advance care planning process more structured and responsive, helping to ensure that the care provided is aligned with the patient’s values and wishes, while increasing efficiency within the healthcare system.
While artificial intelligence (AI) holds great promise for enhancing advance care planning (ACP), its implementation also presents notable challenges that highlight the need for explainable AI (XAI) [21][22]. AI can significantly improve ACP by analyzing large datasets to identify patterns and generate personalized care recommendations that align with individual patient preferences and health conditions [23]. For instance, AI tools can assist healthcare providers in recognizing patients who may benefit from ACP discussions, ensuring that these essential conversations occur promptly [21]. Moreover, by streamlining administrative tasks and providing data-driven insights, AI can enhance the overall efficiency of the healthcare system, allowing providers to focus on patient-centered care [24].
However, despite promising advances in the use of explainable AI (XAI) in healthcare, there is still a significant gap in understanding how XAI can be effectively applied in Advance Care Planning (ACP). Previous studies, such as those by Ghassemi et al. (2021) and Markus et al. (2020) [25][26], have focused only on standard XAI to improve general clinical decision-making, but have not innovatively explored it specifically in ACP . Meanwhile, studies by Yang et al. (2022) and Bienefeld et al. (2023) highlight the benefits of XAI in patient risk prediction but do not discuss how XAI can help bridge communication between patients and healthcare providers regarding care preferences [27][28]. Furthermore, a study by Rane et al. (2023) revealed that although XAI can provide more transparent recommendations, its practical application in advance care planning is still minimal [29].
To address this gap, this study employed a bibliometric analysis of explainable AI (XAI) in advance care planning (ACP). This study aims to identify trends, highlight challenges, and guide the effective integration of XAI in ACP practices. By systematically reviewing the literature, this analysis will provide insights into XAI applications in healthcare, revealing opportunities and barriers to implementation. Additionally, the results will inform stakeholders—including healthcare providers, researchers, and policymakers—about critical areas requiring further exploration. This comprehensive approach will enhance the understanding of XAI's role in healthcare and pave the way for more effective, transparent, and patient-centered advance care planning practices.
The study seeks to present a review of scholarly publications on Explainable AI (XAI) in Advance Care Planning (ACP) over the recent years, from 2019 to 2024. Thus, the following research questions are addressed in this study:
- How has research on Explainable AI in Advance Care Planning evolved intellectually between 2019 and 2024, measured by publications and citations?
- Who are the prominent institutions, nations, and authors in the global research landscape for XAI and ACP?
- Which journals have had the most significant impact on XAI and ACP?
- Which publications have received the most citations or influence in advancing the integration of XAI in ACP?
- What are the patterns of research collaboration and authorship in studies related to XAI and ACP?
- What topics (trendy topics, keywords, keywords pluses, and themes) are associated with the XAI and ACP research field?
The remainder of the paper is structured as follows: Section 2 presents the literature review, Section 3 briefly describes the methods, followed by the results and discussion in Section 4, and finally, Section 5 details the conclusions.
LITERATURE REVIEW
Explainable AI (XAI)
Explainable Artificial Intelligence (XAI) is gaining importance in healthcare, addressing the lack of transparency in AI-based decision-making systems [30][31]. XAI aims to provide clear, understandable explanations for AI predictions, enhancing trust and reliability in high-stakes medical settings [32]. The critical characteristics of XAI include interpretability, transparency, and trustworthiness [33]-[36]. Interpretability in AI healthcare systems refers to the transparency and explainability of AI algorithms, which is crucial for their adoption and trust in clinical settings [37][38]. It involves understanding the relationship between input and output and the ability to explain AI-driven decisions [37]. Transparency ensures that the processes and data underlying AI models are visible and accessible, allowing users to scrutinize the rationale behind decisions [39]. Trustworthiness encompasses both the reliability of the AI outputs and the ethical considerations surrounding their use, as stakeholders must feel confident that AI systems will support rather than undermine patient care [40]. Various models of explainability have been proposed to enhance this understanding, including rule-based systems that provide logical pathways for decision-making, example-based explanations that draw upon previous cases to illustrate outcomes and visual analytics that offer intuitive graphical representations of data [41][42]. These models are particularly vital in healthcare, where clarity can significantly influence treatment decisions and patient outcomes.
Advance Care Planning (ACP)
Advance Care Planning (ACP) is a patient-centred procedure that discusses healthcare preferences, values, and possible future scenarios [10]. Choose a surrogate decision-maker, establish personal values, and document wishes in advance directives [43]. ACP ensures that care aligns with patients' goals, particularly when they lose decision-making capacity [44]. The approach frequently entails several brief chats and should be reviewed as health status changes [10]. Understanding these components is critical for successfully incorporating AI into ACP procedures. AI solutions can facilitate these interactions by offering relevant information and insights based on particular patient situations.
Furthermore, the role of decision-making in Advance Care Planning (ACP) is frequently complex, requiring careful evaluation of ethical and emotional aspects that influence patients' decisions [45]. Theoretical frameworks that address these difficulties might help guide the development and use of AI tools in ACP, ensuring that they complement rather than complicate decision-making [46]. For example, AI may be designed to identify and highlight ethical quandaries or emotional problems during ACP talks, improving overall care quality and ensuring that patients' perspectives are heard and appreciated [47]. Integrating XAI into ACP frameworks improves knowledge and participation while aligning technical breakthroughs with the ethical imperatives of patient-centred care.
Bibliometric Analysis with Biblioshiny
Bibliometric analysis is a systematic method for examining scientific literature to identify patterns, trends, and impact within a field [48]. It utilizes mathematical and statistical tools to measure the interrelationships of publications [49]. This approach is increasingly popular for analyzing large amounts of scientific data [49]. Bibliometric studies typically involve data collection from relevant databases, data cleaning, and application of various bibliometric methods [48]. Key steps include identifying knowledge trends, mapping research collaborations, and exploring the intellectual structure of documents [49]. Biblioshiny, a software tool from R, is used for data analysis in bibliometric studies [50].This method can be applied to evaluate the research output of universities, identify prolific authors, analyze authorship patterns, and determine preferred journals in a field [51]. Bibliometric analysis using tools like Biblioshiny has gained prominence in healthcare research. Recent studies have explored various applications, including the advent of Medical 4.0 technologies [52], decision-making processes in healthcare management [53], and the use of Raspberry Pi in medical applications [51].
Insight Research in XAI and Advance Care Planning
Recent research in eXplainable AI (XAI) has focused on developing methods to enhance the transparency and interpretability of AI systems, particularly in healthcare applications. Post-hoc explanation techniques, including factual, counterfactual, and semi-factual methods, have been explored for image and time-series datasets [54]. Multi-modal and multi-centre data fusion approaches have shown promise in improving XAI for medical applications [55]. A theory-driven, user-centric framework for XAI has been proposed, drawing on insights from philosophy and psychology to address cognitive biases and improve decision-making [56]. In healthcare, advance care planning has been identified as an area where improved communication and understanding of patient preferences are crucial. Research has highlighted the need for more effective planning processes and the importance of considering factors such as the invasiveness of interventions and prognosis in end-of-life care decisions [57].
Collaboration Network Research in XAI and Advance Care Planning
Recent research highlights that interdisciplinary collaboration is crucial for advancing explainable AI (XAI) in healthcare. Specialized conferences foster cross-disciplinary exchange and drive XAI innovation [58]. Bibliometric analysis reveals that XAI research in healthcare has gained momentum since 2011, with the USA, China, and Canada leading in publications [59]. Similarly, research on advance care planning (ACP) has increased significantly over the past three decades, with North America, Western Europe, and Australia being the most productive regions [60]. Human-AI collaboration in healthcare shows promise in addressing workforce shortages and improving care quality, but challenges remain, including bias investigation, trust issues, and adoption barriers [61]. These studies underscore the importance of collaborative efforts in developing effective XAI solutions for healthcare applications, including ACP.
Future Impacts Research in XAI and Advance Care Planning
Explainable Artificial Intelligence (XAI) is gaining prominence in healthcare, addressing the critical need for transparency in AI-driven clinical decision support systems [52]. XAI enhances clinician confidence, improves decision-making, and increases system trustworthiness [29][52]. It is precious in specialities like radiology, pathology, cardiology, and oncology, where interpretable models can elucidate complex diagnoses and treatment recommendations [29].
In advance care planning (ACP), XAI can play a transformative role by facilitating more transparent communication between healthcare providers and patients, especially when navigating intricate end-of-life decisions. However, the implementation of XAI in healthcare faces challenges, including the need for ethical considerations, fairness, and accountability [53]. Responsible AI development is crucial to ensure equitable and ethical use across diverse global regions, particularly in ACP scenarios where disparities in healthcare access may be pronounced.
While XAI aims to make AI algorithms understandable to humans, thereby increasing trust in healthcare applications, alternative approaches to build confidence in AI systems are also being explored [32]. Future research should focus on developing specific tools and frameworks that enhance the integration of XAI in ACP, ensuring that these technologies effectively support patient-centred decision-making and align with ethical standards in healthcare.
METHODS
This study applied bibliometric analysis to systematically examine the scientific literature on applying Explainable Artificial Intelligence (XAI) in advance care planning (ACP). This method offers insight into study trends, collaborative networks between researchers, and thematic focuses in XAI and ACP by analyzing publication practices, citation networks, and keyword frequencies. This study aims to identify recent developments, challenges, and opportunities for XAI integration in advance care planning.
Data Source and Strategy
In this study, the method used is bibliometric analysis based on knowledge publications using the topics of XAI and Advance Care Planning. The data for this bibliometric analysis was retrieved from the Scopus database on November 22, 2024. Data retrieval in this study was taken from the Scopus database. This study uses the Scopus database as the main primary data source [62][63]. Scopus was chosen for this study because of its comprehensive features, broad coverage, guaranteed integrity, strong citation base, and data standards consistent with continuous analysis [62]. This study used the criteria below to collect publication data and utilized a particular query in Scopus. [62][64][65]. The search query was designed to capture publications at the intersection of Explainable Artificial Intelligence (XAI) and Advance Care Planning (ACP). The Boolean query used was ( TITLE-ABS-KEY ( "Advance Care Planning" ) OR TITLE-ABS-KEY ( "Advance Care Plan" ) OR TITLE-ABS-KEY ( "Advance directive" ) OR TITLE-ABS-KEY ( "palliative care" ) AND TITLE-ABS-KEY ( "Explainable Artificial Intelligence" ) OR TITLE-ABS-KEY ( "Explanaible AI" ) OR TITLE-ABS-KEY ( "artificial intelegence" ) OR TITLE-ABS-KEY ( "AI" ) OR TITLE-ABS-KEY ( "Machine Learning" ) ) AND PUBYEAR > 2018 AND PUBYEAR < 2025 AND ( LIMIT-TO ( LANGUAGE , "English" ) ) AND ( LIMIT-TO ( SRCTYPE , "j" ) ) AND ( LIMIT-TO ( DOCTYPE , "ar" ) ) can be seen in Table 1.
Table 1. Boolean Query for This Study
Construct | Search key terms |
AI-XAI related terms | ( "Explainable Artificial Intelligence" ) OR TITLE-ABS-KEY ( "Explanaible AI" ) OR TITLE-ABS-KEY ( "artificial intelegence" ) OR TITLE-ABS-KEY ( "AI" ) OR TITLE-ABS-KEY ( "Machine Learning" ) |
Advance Care Planning related terms | ( TITLE-ABS-KEY ( "Advance Care Planning" ) OR TITLE-ABS-KEY ( "Advance Care Plan" ) OR TITLE-ABS-KEY ( "Advance directive" ) OR TITLE-ABS-KEY ( "palliative care" ) |
Document type | Article |
Language | English |
Period | 2019-2024 |
The choice of keywords in this query was deliberate and strategic. The terms "Advance Care Planning," "Advance Care Plan," "Advance Directive," and "Palliative Care" were included to ensure that the analysis captures literature related to critical aspects of patient care and decision-making in healthcare settings. These concepts are central to understanding how advance care discussions can be enhanced through technological interventions.
Additionally, the inclusion of "Explainable Artificial Intelligence," "Explainable AI," "Artificial Intelligence," "AI," and "Machine Learning" reflects the focus on the technological frameworks that underpin XAI. These keywords are essential for examining how AI technologies can improve transparency and understanding in healthcare decisions, which is particularly important in palliative and end-of-life care contexts.
Boolean operators (AND, OR) allowed for a comprehensive search strategy that captures a wide range of publications while ensuring that only relevant studies at the intersection of XAI and ACP are included. The temporal focus, set to include publications from 2018 to 2025, ensures that the analysis reflects the most recent trends and developments in the field, while language and document type restrictions guarantee that the analysis is based on high-quality, peer-reviewed English-language articles. Through this targeted approach, the study aims to provide a thorough overview of the current research landscape, identifying key trends and future directions in this vital area of healthcare.
Inclusion and Exclusion Criteria
An explicit inclusion and exclusion criteria were established to maintain the quality and relevance of the publications included in the analysis for this study. The inclusion criteria focused on articles related to explainable artificial intelligence (XAI) and Advance Care Planning (ACP). This study restricted the publication period to 2019 and 2024. This period was chosen because it aligns with significant advancements in artificial intelligence technologies and methodologies, particularly in healthcare applications. Grey literature, conference proceedings, and books or book chapters were excluded from the study, as were publications in languages other than English. This restriction ensured that the collected research reflected the most recent developments in the field, given that technologies and methodologies in artificial intelligence continue to evolve rapidly. Focusing on publications within this period allowed this study to capture the latest trends, challenges, and innovations in applying Explainable AI to Advance Care Planning.
Furthermore, selecting English-language documents allowed access to broader literature, given that many international studies and leading publications in the field are often published in English. This restriction ensured that the collected research reflected the most recent developments in the field, given that technologies and methodologies in artificial intelligence continue to evolve rapidly based on factors such as peer-review status, publication in English, and direct relevance to the research topic. In contrast, exclusion criteria targeted articles not available in full text, conference proceedings, book chapters, or publications that did not directly address the application of explainable AI in advanced care planning or related fields. This systematic approach to article selection helped the study focus the analysis on the most impactful and informative literature.
Bibliometric Analysis
The bibliometric analysis involved the examination of various indicators, including publication trends, citation analysis, author productivity, institutional collaboration, and keyword co-occurrence [51]-[53]. These metrics were used to gain insights into the research landscape, important contributors, and emerging trends in the field [53][54]. This study utilized the Biblioshiny’s web application, which is a user-friendly interface for the Bibliometric R package, to conduct the bibliometric analysis [55]-[57] . This software allowed for the visualization and interpretation of the data, enabling this study to identify publication patterns, collaboration networks, influential authors and institutions, and the conceptual structure of the research domain.
Biblioshiny has proven effective in various contexts; for instance, it has been used to analyze healthcare applications, revealing increased research over time and identifying trending topics [66]. Additionally, it has been employed to study wearable devices in healthcare services, successfully identifying prominent sources, authors, and trending topics [67]. Biblioshiny has mapped scientific production on organizational tensions in organizational research, highlighting influential authors, countries, and journals [50].
RESULT AND DISCUSSIONS
Publication Trends
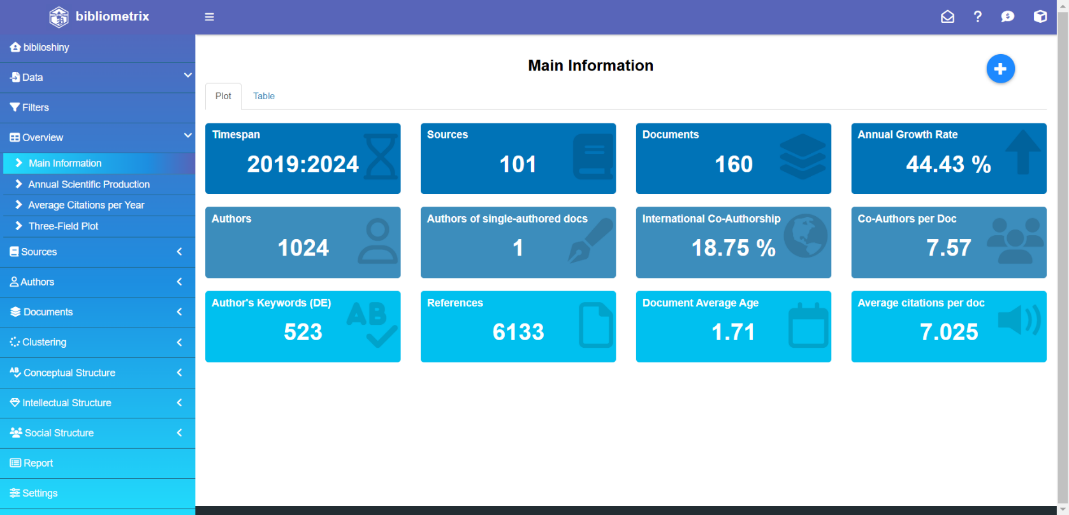
The data presented in Figure 1 and Table 2 provide a comprehensive overview of the critical characteristics and metrics of the dataset analyzed in this study. The time span covered spans from 2019 to 2024, encompassing a period of significant research activity and evolution in the field. The study draws upon 101 distinct sources, ranging from scholarly journals to books and other publications, to inform the analysis of 160 documents.
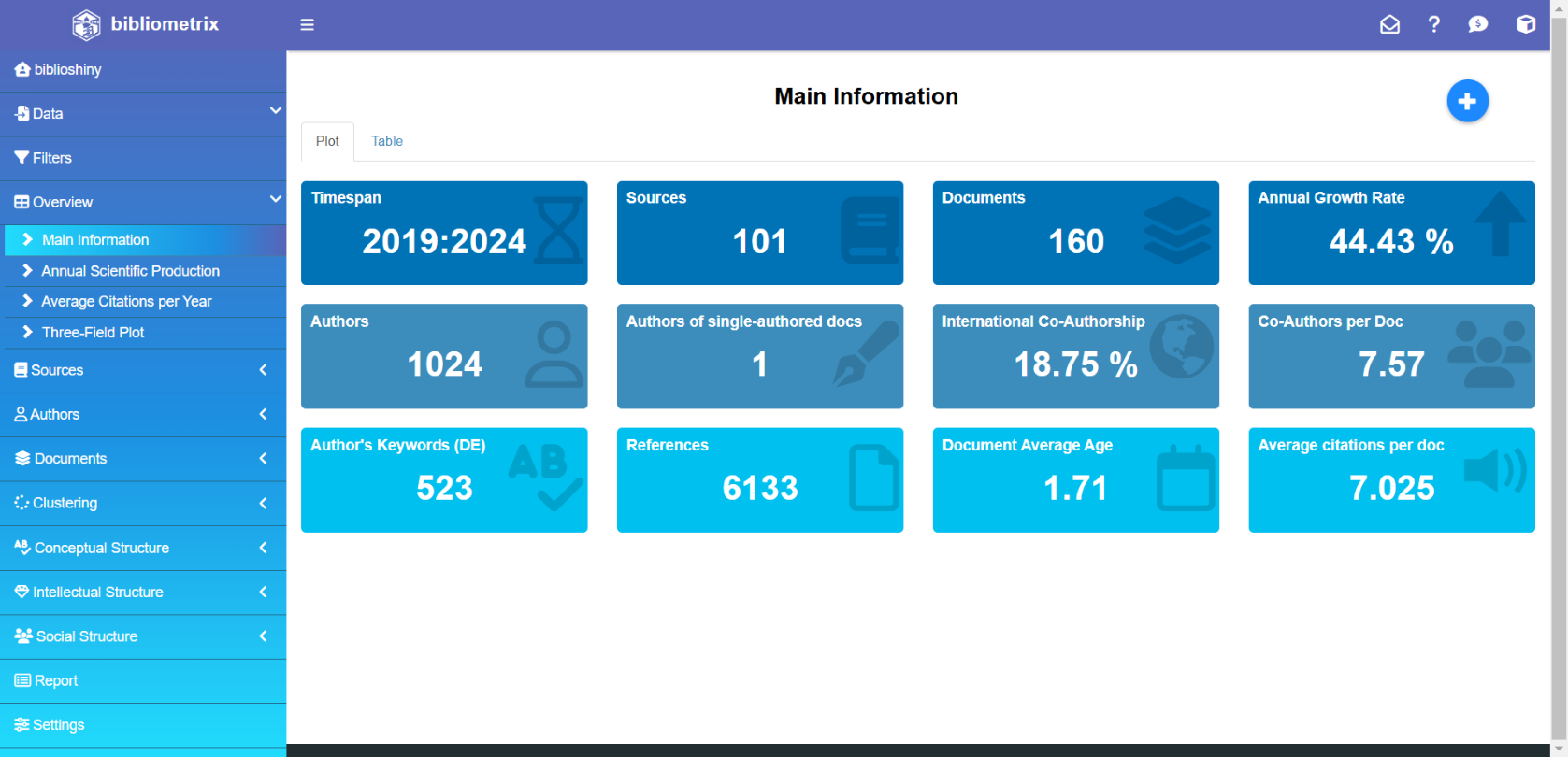
Figure 1. Main Information for this study
As shown in Figure 1, the literature's impressive annual growth rate of 44.43% underscores the research landscape's dynamic and rapidly evolving nature. The documents' average age of 1.71 years suggests a focus on cutting-edge and timely research, while the high average number of citations per document, at 7.025, underscores the work's significant impact and influence within the scholarly community.
Delving into the documents' content, the analysis reveals 1.489 Keywords Plus (ID) and 523 Author's Keywords (DE), as shown in Table 2. This rich keyword corpus provides a detailed understanding of the key concepts, themes, and areas of exploration within the literature, serving as a valuable starting point for thematic analyses and identifying emerging trends.
Annual Publication Counts
In Figure 1 of this study, the average age of the documents is 1.71 years, indicating that most of the literature is relatively recent and reflects current trends and advancements in explainable AI (XAI) and advance care planning (ACP) research. Each document has an average of approximately 7.025 citations, contributing to 6.133 citations across the dataset. The analysis also revealed a rich diversity in keyword usage, with 1.489 Keywords Plus and 523 author-defined keywords, highlighting the wide range of topics explored within the literature. The authorship landscape consists of contributions from 1.024 distinct authors, with only one document being authored by a single individual, underscoring the collaborative nature of research in this area. On average, each document has 7.57 co-authors, and 18.75% of the documents result from international collaborations, emphasizing the global interest and cooperative efforts in this research domain. Notably, all identified documents are articles that strongly focus on disseminating findings through peer-reviewed channels.
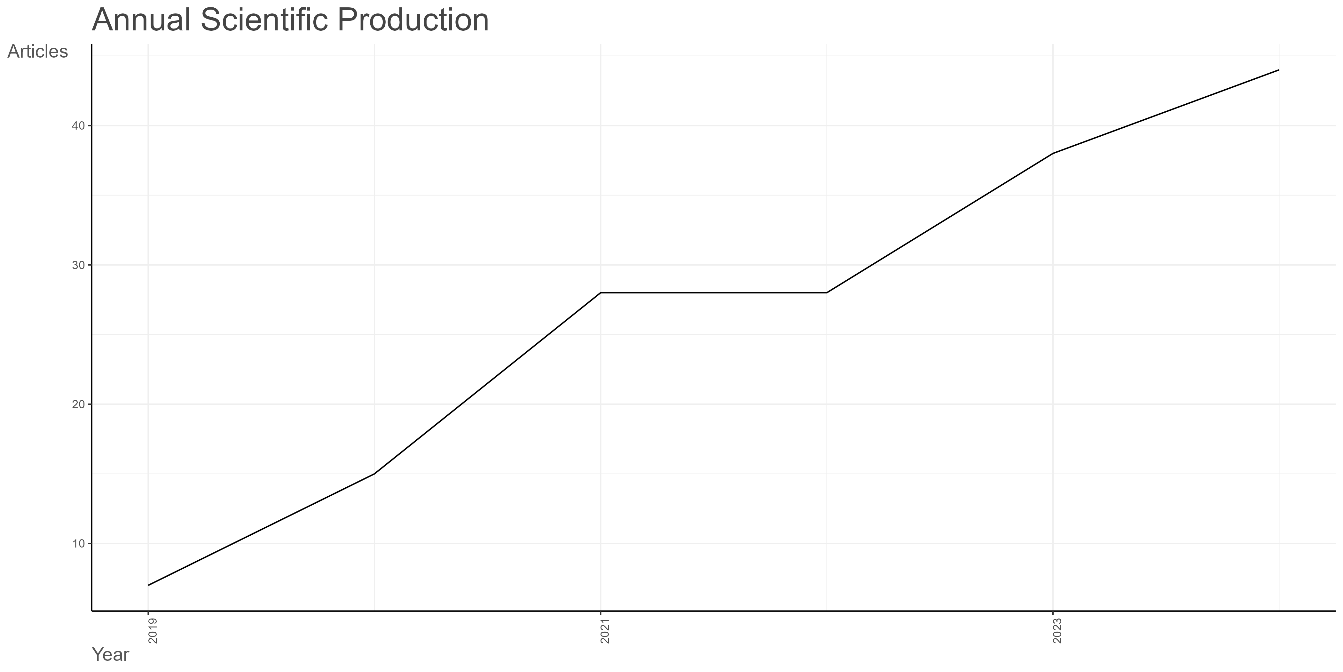
Figure 2. Publication Trend on Explainable AI and Advance Care Planning
The annual number of publications, illustrated in Figure 2, demonstrates a steady increase: in 2019, only 7 articles were published, which rose to 15 in 2020. This momentum continued, with 28 articles published in 2021 and 2022, followed by a significant rise to 38 in 2023 and 44 in 2024. This upward trend indicates a growing body of literature and an increasing recognition of the relevance of XAI in enhancing the advance care planning process.
The authorship landscape involves 1.024 individual authors, with a single-authored document representing one of the 160 documents analyzed. Table 2 highlights the collaborative nature of the research, with an average of 7.57 co-authors per document. Furthermore, 18.75% of the documents involve international co-authorship, showcasing the global and interdisciplinary nature of the scholarly community in this domain.
Lastly, the document types are exclusively research articles, as indicated in Table 2. This suggests a focused and rigorous approach to investigating the research questions and objectives. This homogeneity in the document types allows for a more consistent and meaningful literature analysis.
Table 2. Summary statistics of the articles collected
Description | Results |
MAIN INFORMATION ABOUT DATA |
Timespan | 2019:2024 |
Sources (Journals, Books, etc) | 101 |
Documents | 160 |
Annual Growth Rate % | 44.43 |
Document Average Age | 1.71 |
Average citations per doc | 7.025 |
References | 6133 |
DOCUMENT CONTENTS |
Keywords Plus (ID) | 1489 |
Author's Keywords (DE) | 523 |
AUTHORS |
Authors | 1024 |
Authors of single-authored docs | 1 |
AUTHORS COLLABORATION |
Single-authored docs | 1 |
Co-Authors per Doc | 7.57 |
International co-authorships % | 18.75 |
DOCUMENT TYPES |
article | 160 |
Key Contributors to the Field
Prominent Intitutions
The trends across the top 10 most relevant institutions provide valuable insights into the productivity research and growth in this field over time. As shown in Figure 3 for this study, The University of Pennsylvania stands out as the top contributor, with an impressive 85 articles. This firmly establishes the university as a powerhouse for research and scholarly productivity.
Following closely, the Stanford University School of Medicine has produced 40 articles, demonstrating its significant influence and active engagement in this area of study. The University of Vermont comes in third place with 32 published works. Prominent medical institutions like Harvard Medical School and Mayo Clinic have also made substantial contributions, with 21 and 19 articles, respectively. This reflects the strong involvement of specialized healthcare organizations in the research efforts.
Figure 3. Most relevant affiliations
Other notable entities include the University of Utah, Vanderbilt University Medical Center, Stanford University, the University of California, and the University of Washington, each contributing 12 to 14 articles. The diversity of these top affiliations, encompassing renowned universities and specialized medical centers, underscores the collaborative and interdisciplinary nature of the research. This publication landscape suggests a vibrant and dynamic ecosystem driving advancements in the field.
Influential Nations
In this study, the United States is the leading contributor to research in this field, with 673 publications (see Table 3). Germany follows with 71 publications, while China and Canada contribute 51 and 47, respectively. Other notable contributors include Japan (38), Italy (36), the United Kingdom (29), Australia (28), the Netherlands (26), and France (25). This data indicates a global interest in this research area, with significant activity concentrated in North America, Europe, and Asia.
Additionally, countries like India and Switzerland each have 20 publications, while Spain (18), Singapore (14), and South Korea (13) further demonstrate the expanding reach and interest in this field. The diverse geographic representation, with contributions from countries across Europe, Asia, North America, South America, and the Middle East, suggests a global effort to explore and understand the research topic.
The analysis highlights the United States as the dominant force in this field. However, it also reveals substantial involvement from other major economies and scientific powerhouses worldwide, underscoring the international collaboration and engagement within this scientific domain.
Table 3. Top Countries by Scientific Publications
Region | Freq | Region | Freq |
USA | 673 | INDIA | 20 |
GERMANY | 71 | SWITZERLAND | 20 |
CHINA | 51 | SPAIN | 18 |
CANADA | 47 | SINGAPORE | 14 |
JAPAN | 38 | SOUTH KOREA | 13 |
ITALY | 36 | SWEDEN | 11 |
UK | 29 | COLOMBIA | 10 |
AUSTRALIA | 28 | NORWAY | 10 |
NETHERLANDS | 26 | TURKEY | 10 |
FRANCE | 25 |
|
|
Notable Authors Contributing to XAI and ACP Research
In this study, several prominent authors regularly emerged as the most productive, showcasing their substantial contributions to advancing and implementing explainable AI in advance care planning. Figure 4 demonstrates that these ten authors provide substantial research on this subject, showcasing their knowledge and commitment to increasing the comprehension and application of explainable AI in advanced care planning. Dr. RB Parikh is at the top of the list with nine publications, closely followed by Dr. C Chivers with 7. Dr. N O'Connor, Dr. MS Patel, Dr. LM Schuchter, and Dr. LN Shulman each authored five papers, demonstrating their substantial contributions to the subject. Additional notable authors include Dr. SW Asai, Dr. V Blanes-Selva, Dr. J Chen, and Dr. JM García-Gómez, each with four publications.
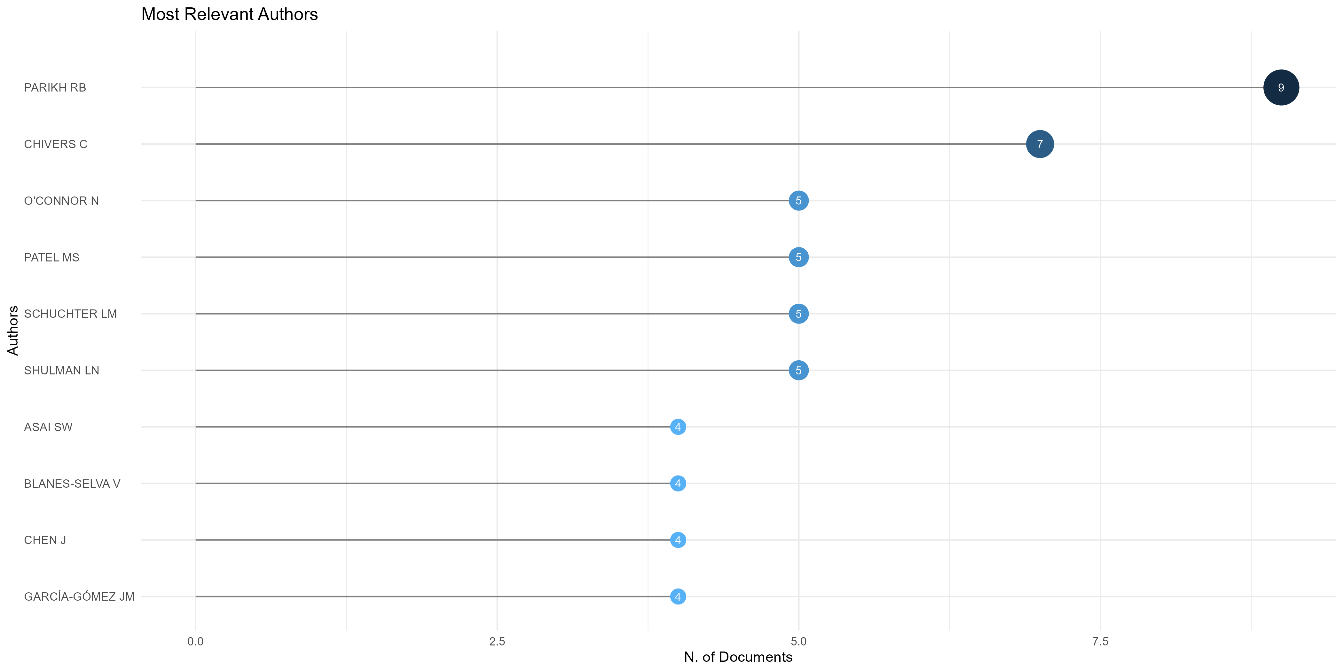
Figure 4. Ten most relevant authors
In addition to the above information, Author Impact Analysis is essential in understanding an individual’s contribution to research in this field. The Table 4 presents some of the leading authors along with metrics that illustrate their influence:
Table 4. Author local impact
Element | h_index | g_index | m_index | TC | NP | PY_start |
PARIKH RB | 7 | 9 | 1.400 | 132 | 9 | 2020 |
CHIVERS C | 6 | 7 | 1.200 | 117 | 7 | 2020 |
O'CONNOR N | 5 | 5 | 1.000 | 114 | 5 | 2020 |
CHEN J | 4 | 4 | 0.800 | 91 | 4 | 2020 |
MANZ CR | 4 | 4 | 0.800 | 100 | 4 | 2020 |
PATEL MS | 4 | 5 | 0.800 | 104 | 5 | 2020 |
SCHUCHTER LM | 4 | 5 | 0.800 | 106 | 5 | 2020 |
SHULMAN LN | 4 | 5 | 0.800 | 106 | 5 | 2020 |
ASAI SW | 3 | 4 | 0.750 | 37 | 4 | 2021 |
BEKELMAN JE | 3 | 3 | 0.600 | 88 | 3 | 2020 |
Journal Impact
This study's analysis of publication output highlights several vital journals that have significantly contributed to the literature on Explainable AI (XAI) in advance care planning (see Figure 5). The Journal of Pain and Symptom Management leads with 11 articles, emphasizing its essential role in disseminating research related to symptom management in palliative care. The Journal of Palliative Medicine has published eight articles that highlight the importance of palliative approaches in healthcare settings.
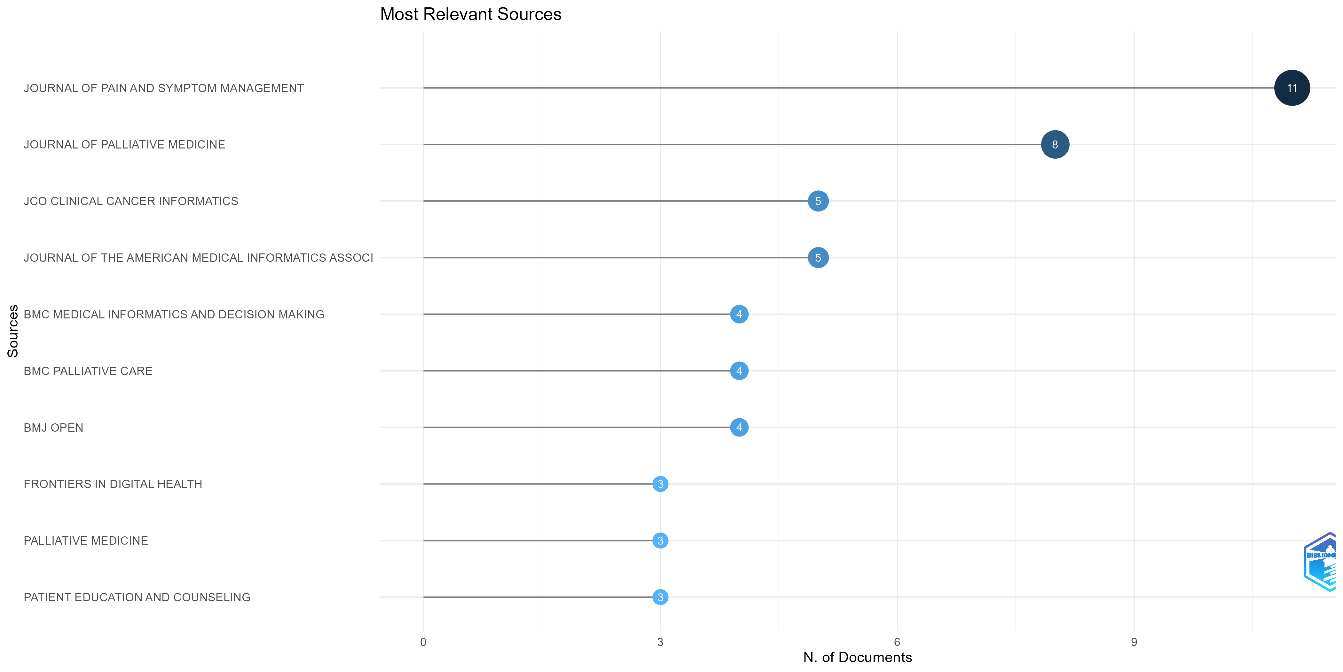
Figure 5. Most relevant sources
Other notable journals include JCO Clinical Cancer Informatics and the Journal of the American Medical Informatics Association, each contributing five articles that reflect the intersection of cancer care and informatics. Additionally, BMC Medical Informatics and Decision Making, BMC Palliative Care, and BMJ Open have each published four articles, emphasizing their contributions to medical decision-making and palliative care research. Lastly, journals such as Frontiers in Digital Health, Palliative Medicine, and Patient Education and Counseling have each contributed three articles, indicating a growing interest in digital health solutions and patient-centered care approaches within the context of advance care planning. These journals are crucial platforms for advancing knowledge and practice in integrating XAI into healthcare.
In addition to their overall contributions, an analysis based on Bradford's Law (see Figure 6) reveals the core sources that significantly shape the discourse on XAI in advance care planning. The Journal of Pain and Symptom Management ranks first with 11 articles, followed by the Journal of Palliative Medicine, with eight articles categorized in Zone 1, indicating their central role in this research area. Other prominent journals in this zone include JCO Clinical Cancer Informatics and the Journal of the American Medical Informatics Association, each contributing five articles. Additionally, BMC Medical Informatics and Decision Making, BMC Palliative Care, and BMJ Open each published four articles, reinforcing their relevance in medical informatics and palliative care. Lastly, journals such as Frontiers in Digital Health, Palliative Medicine, and Patient Education and Counselling contributed three articles, further highlighting the broad interest in digital health solutions and patient-centered care.
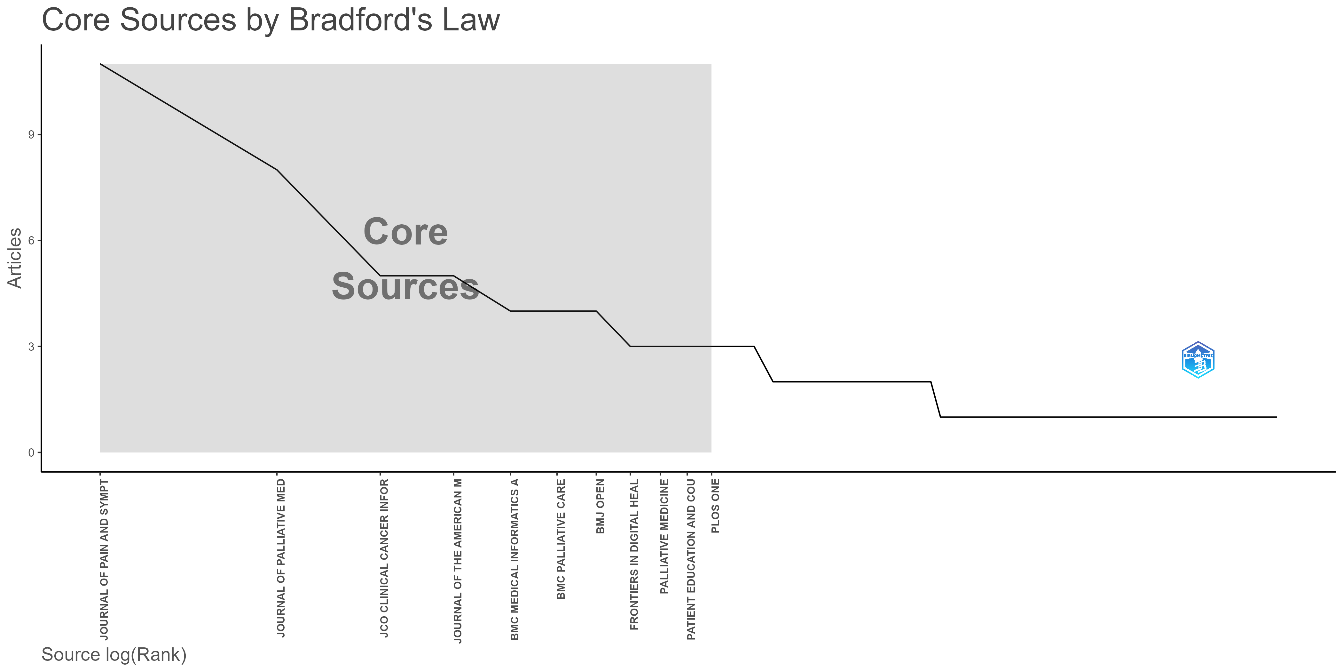
Figure 6. Core Sources by Bradford's Law
The local impact of these journals is further clarified through the analysis of key metrics presented in Table 5, such as h-index, g-index, and total citations (TC). The Journal of Pain and Symptom Management stands out with an h-index of 5 and 74 citations, indicating significant influence and productivity in the field, particularly with 11 articles published since 2021. Similarly, the Journal of the American Medical Informatics Association has an h-index of 4, with 59 citations from five articles published since 2021, demonstrating its importance in medical informatics.
Table 5. Sources' Impact
Element | h_index | g_index | m_index | TC | NP | PY_start |
JOURNAL OF PAIN AND SYMPTOM MANAGEMENT | 5 | 8 | 1.250 | 74 | 11 | 2021 |
JOURNAL OF THE AMERICAN MEDICAL INFORMATICS ASSOCIATION | 4 | 5 | 1.000 | 59 | 5 | 2021 |
BMC MEDICAL INFORMATICS AND DECISION MAKING | 3 | 4 | 0.500 | 55 | 4 | 2019 |
JCO CLINICAL CANCER INFORMATICS | 3 | 4 | 0.750 | 24 | 5 | 2021 |
PALLIATIVE MEDICINE | 3 | 3 | 0.500 | 84 | 3 | 2019 |
PATIENT EDUCATION AND COUNSELING | 3 | 3 | 0.600 | 27 | 3 | 2020 |
BMC PALLIATIVE CARE | 2 | 4 | 0.400 | 24 | 4 | 2020 |
BMJ OPEN | 2 | 4 | 0.333 | 30 | 4 | 2019 |
BMJ SUPPORTIVE AND PALLIATIVE CARE | 2 | 2 | 0.400 | 26 | 2 | 2020 |
HEALTH INFORMATICS JOURNAL | 2 | 2 | 0.500 | 11 | 2 | 2021 |
An analysis of article production over time reveals significant trends in the contributions of critical journals to the literature on XAI in advance care planning (see Figure 7). The Journal of Pain and Symptom Management has shown an extraordinary output increase, from no publications in 2019 to 11 articles in 2024. This upward trajectory emphasizes the journal's vital role in addressing critical issues in symptom management.
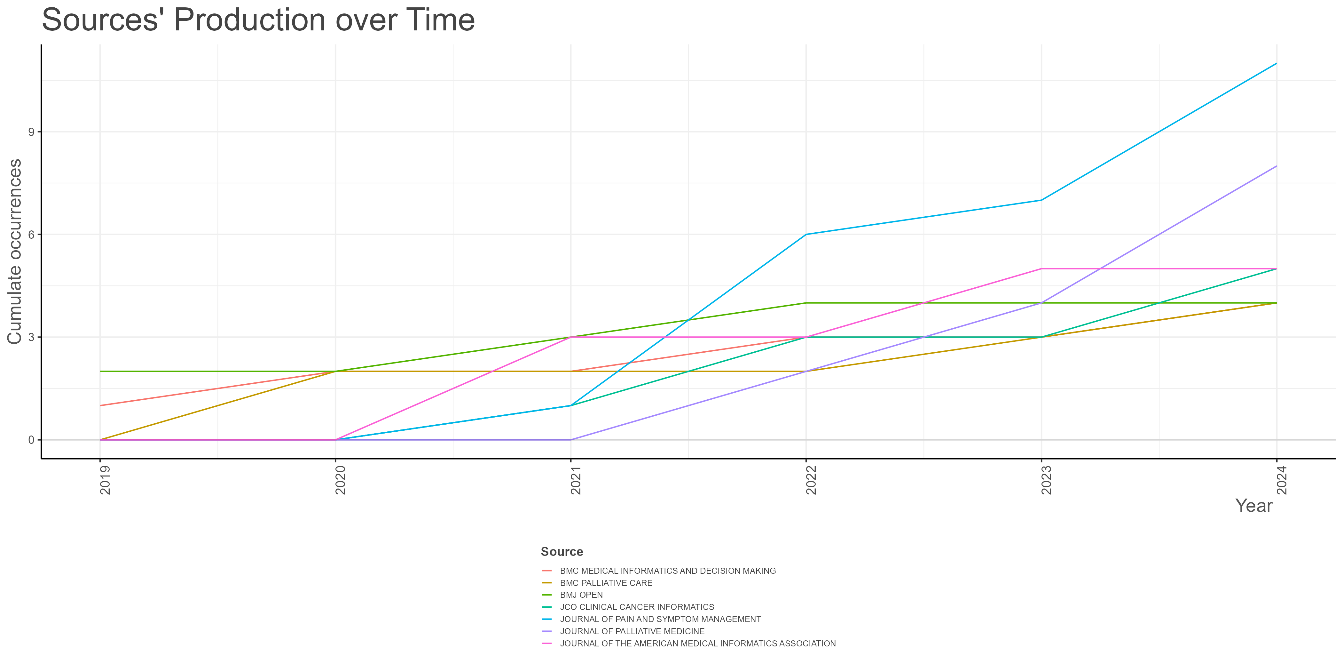
Figure 7. Sources' Production over Time
Likewise, the Journal of Palliative Medicine has consistently increased its publications, producing eight articles in 2024, up from two articles in 2022. This reflects the growing importance of palliative care research in the context of XAI and advance care planning.
JCO Clinical Cancer Informatics and the Journal of the American Medical Informatics Association have also maintained stable contributions, each producing five articles in 2024, affirming their relevance at the intersection of cancer care and medical informatics. Other journals, such as BMC Medical Informatics and Decision Making and BMC Palliative Care, have shown variability in publication numbers, each contributing four articles in 2024. Conversely, BMJ Open remains active with four articles, reflecting its commitment to advancing medical research.
The data indicates a growing momentum in this field, particularly from 2021 onward, with a notable spike in publications across most journals in 2022 and 2024. This surge in research output suggests an increasing recognition of the importance of integrating explainable AI into advance care planning and palliative care as researchers strive to enhance understanding and application in clinical settings.
Finally, the production trends across these journals emphasize their critical role in academic discourse and highlight the evolving landscape of research focused on XAI in healthcare. These journals will likely remain central to advancing knowledge and practice in this vital area as this field develops.
Highly Cited Publications
Based on the information in the Table 6 and Figure 8, this section will discuss the most highly cited publications globally related to research on Explainable AI (XAI) in advance care planning. At the top of the list is the article "MANZ CR, 2020, JAMA ONCOL," which has received 69 global citations, an average of 13.8 citations per year, and a normalized citation score of 4.42 [68]. This article demonstrates a significant impact in the field. Following it is the article "GHORAANI B, 2021, BIOMED SIGNAL PROCESS CONTROL," which has received 57 global citations, with an average of 14.25 citations per year and a normalized citation score of 5.10. This article also shows a strong influence in the field of medical signal processing related to XAI.
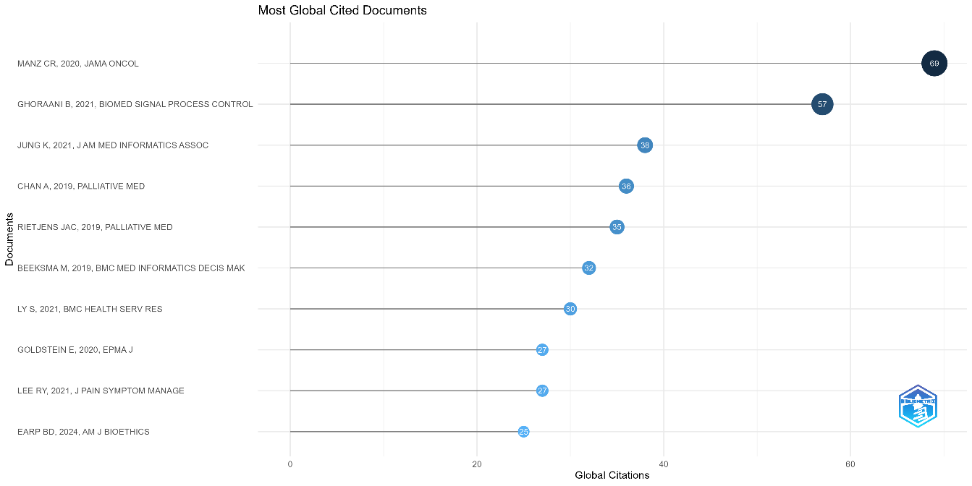
Figure 8. Most Global Cited Documents
Next, the article "JUNG K, 2021, J AM MED INFORMATICS ASSOC" has received 38 global citations, an average of 9.5 per year, and a normalized citation score of 3.40 [69]. This article reflects an essential contribution to medical informatics. Other publications that make the list of the top 10 most cited include those from the journals "Palliative Medicine," "BMC Medical Informatics and Decision Making," "BMC Health Services Research," "EPMA Journal," and "American Journal of Bioethics." This indicates the broad scope of topics related to integrating XAI in advance care planning, encompassing palliative aspects, medical informatics, decision-making, and ethical considerations.
Table 6. Highly Cited Publications on Explainable AI in Advance Care Planning
Paper | DOI | Total Citations | TC per Year | Normalized TC |
MANZ CR, 2020, JAMA ONCOL | 10.1001/jamaoncol.2020.4331 | 69 | 13.80 | 4.42 |
GHORAANI B, 2021, BIOMED SIGNAL PROCESS CONTROL | 10.1016/j.bspc.2020.102249 | 57 | 14.25 | 5.10 |
JUNG K, 2021, J AM MED INFORMATICS ASSOC | 10.1093/jamia/ocaa318 | 38 | 9.50 | 3.40 |
CHAN A, 2019, PALLIATIVE MED | 10.1177/0269216318810421 | 36 | 6.00 | 1.70 |
RIETJENS JAC, 2019, PALLIATIVE MED | 10.1177/0269216318824275 | 35 | 5.83 | 1.66 |
BEEKSMA M, 2019, BMC MED INFORMATICS DECIS MAK | 10.1186/s12911-019-0775-2 | 32 | 5.33 | 1.51 |
LY S, 2021, BMC HEALTH SERV RES | 10.1186/s12913-021-06934-y | 30 | 7.50 | 2.68 |
GOLDSTEIN E, 2020, EPMA J | 10.1007/s13167-020-00221-2 | 27 | 5.40 | 1.73 |
LEE RY, 2021, J PAIN SYMPTOM MANAGE | 10.1016/j.jpainsymman.2020.08.024 | 27 | 6.75 | 2.42 |
EARP BD, 2024, AM J BIOETHICS | 10.1080/15265161.2023.2296402 | 25 | 25.00 | 17.19 |
This list of publications provides a comprehensive overview of the most influential research works that serve as critical references in XAI and advance care planning. These publications have significantly contributed to advancing knowledge and practice integrating XAI into healthcare.
Collaboration Network
Co-Authorship Analysis
Figure 9 presents the co-authorship network for this research landscape, revealing several distinct clusters or groups of researchers who have collaborated closely with one another. One prominent cluster is the purple cluster centred around the researchers "Parikh RB" and "Schuchter LM". This cluster appears relatively isolated from the other groups in the network, with few direct connections to the researchers in other coloured clusters. This suggests that the researchers in this purple cluster may be focused on a more specialized or niche area of research compared to the broader collaborative efforts observed in the other parts of the network.
In contrast, the blue cluster seems the largest and most central, with researchers like "Zhang H" and "Bates DW" having high betweenness centrality. This indicates that these researchers play a crucial role in facilitating knowledge exchange and collaboration between the different research groups represented in the network. The green cluster includes researchers like "Blanes-Selva" and "Garcia-Gomez JM", who have relatively high closeness centrality, suggesting they are well-connected. The orange cluster, on the other hand, appears to have fewer internal connections but may serve as a bridge between larger central clusters.
Overall, the structure of this co-authorship network reflects a diverse and multi-faceted research landscape, with some specialized sub-communities and, more broadly, collaborative efforts across the field. Further investigation into each cluster's specific research topics and contributions could provide additional insights into the dynamics and evolving patterns of this collaborative ecosystem.
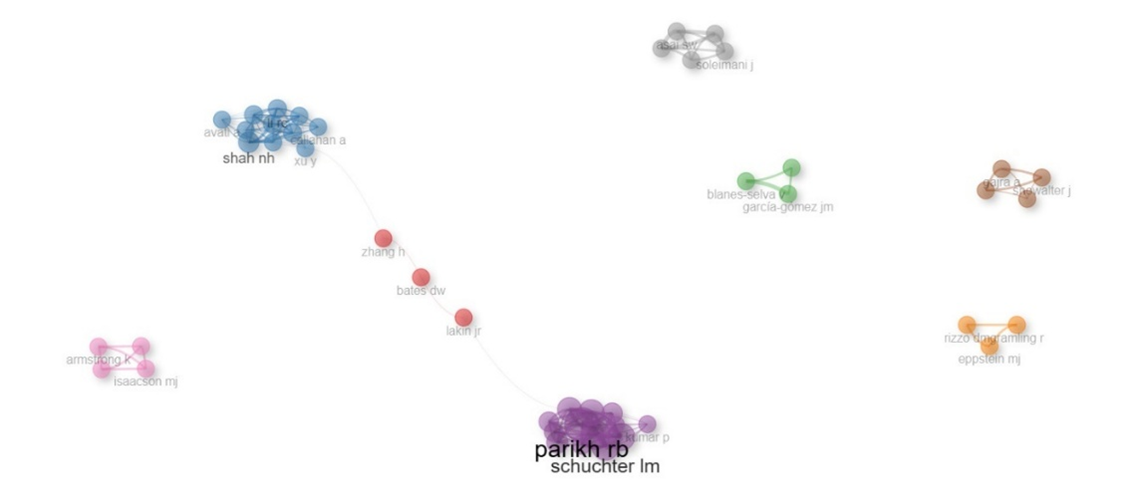
Figure 9. Collaboration Network among Authors
Institutional Collaborations
Figure 10 presents a comprehensive visual representation of the extensive institutional collaborations and connections centred around Harvard Medical School. From an observational standpoint, the image paints a compelling picture of the school's pivotal role as a central hub within the broader medical ecosystem.
The network mapping reveals that Harvard Medical School has established a robust and diverse array of partnerships with prominent medical institutions, including the Massachusetts General Hospital, the University of Pennsylvania, the Dana-Farber Cancer Institute, the University of Washington, and the Stanford University School of Medicine. These collaborative linkages suggest that the school plays a critical role in facilitating the exchange of knowledge, resources, and expertise across this interconnected landscape.
By occupying this central position, Harvard Medical School leverages its extensive network to drive innovation, advance research initiatives, and enhance educational opportunities in the pursuit of improving healthcare outcomes. The intricate web of relationships depicted in the image underscores the collaborative nature of the medical field, where interdisciplinary and inter-institutional cooperation is essential for addressing complex challenges and driving progress.
The centrality of Harvard Medical School within this network highlights its influential role and ability to catalyze collaborative efforts across the broader medical ecosystem. This strategic positioning allows the institution to harness the collective capabilities of its affiliated partners, fostering synergies that can be harnessed to tackle the multifaceted issues faced in human health and well-being.
The visual mapping provided in Figure 8 offers a comprehensive and holistic perspective on the institutional collaborations that shape the medical landscape. This analysis provides valuable insights that can inform strategic decision-making and guide the development of effective collaboration frameworks within the industry, ultimately contributing to advancing medical research, education, and patient care.
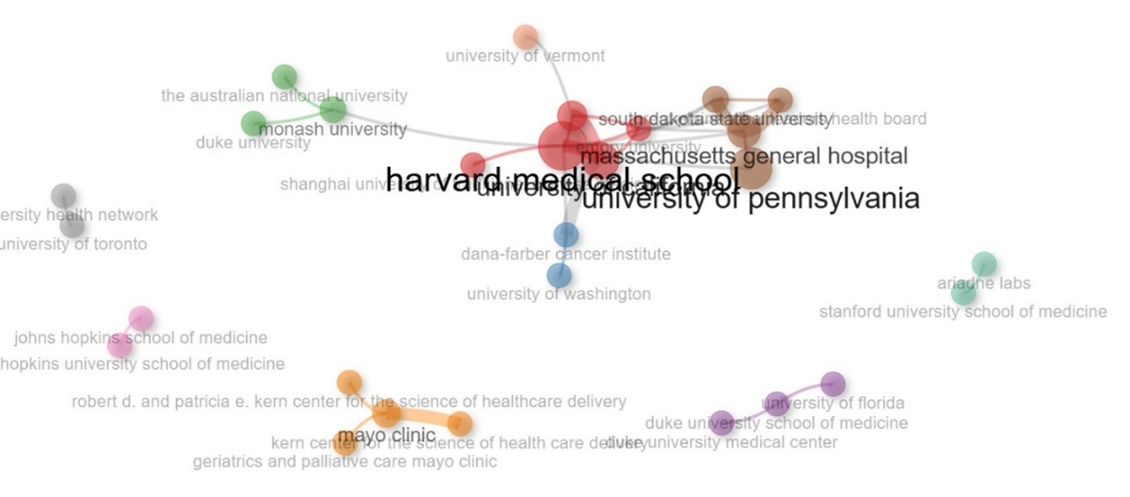
Figure 10. Institutional Collaborations Network
International Collaborations Dynamics
The visual representation in Figure 11 represents a compelling picture of the international collaboration dynamics within this research ecosystem. The network mapping reveals a complex web of interconnections between various countries and regions, showcasing the work's global reach and collaborative nature.
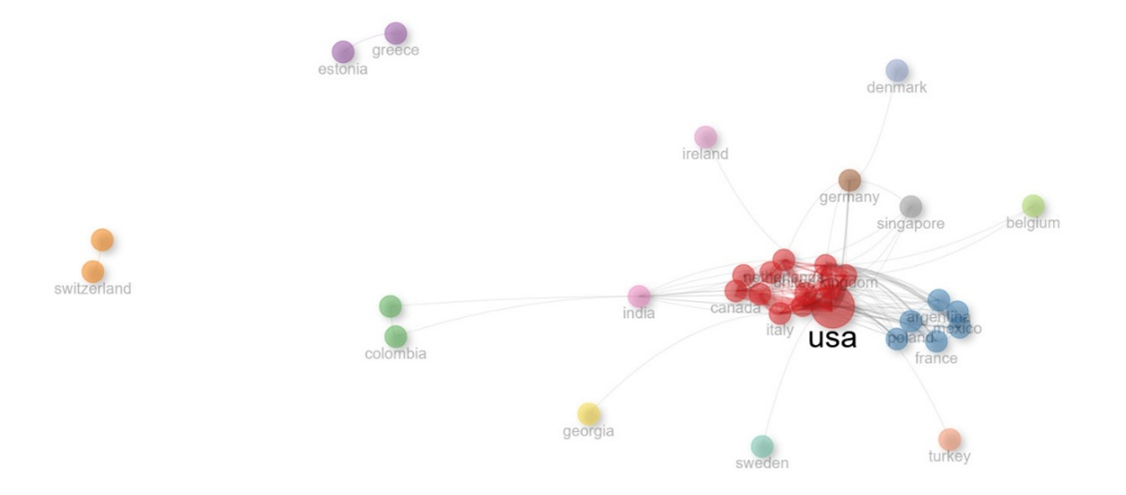
Figure 11. Countries Collaboration Network
The United States (USA) emerges as a dominant player at the centre of this network, serving as a hub for many international partnerships. The dense cluster of connections radiating from the USA node suggests it is pivotal in facilitating and coordinating collaborative efforts across national boundaries.
Surrounding the USA, prominent countries and regions, such as Canada, Italy, Argentina, Mexico, France, and Colombia, are actively engaged in this global collaborative network. The varying sizes and colours of the nodes indicate the differing intensities and specializations of these international partnerships.
For instance, larger nodes like India and the United Kingdom (UK) have relatively more influential roles and active involvement within this ecosystem. The connections between these central nodes and the smaller satellite nodes, such as Greece, Estonia, Denmark, and Singapore, suggest the presence of diverse collaborative relationships, potentially spanning different research domains or areas of expertise.
This intricate structure highlights the dynamic and multifaceted nature of international collaborations in the field of study. These global linkages enable the cross-pollination of ideas, the sharing of resources and expertise, and the collective advancement of international research, innovation, and knowledge dissemination.
By examining the patterns and structures of this international collaboration network, researchers and policymakers can gain valuable insights into the existing collaborative landscape, identify potential areas for further strengthening international partnerships, and leverage these insights to foster a more robust and interconnected global research ecosystem.
The visual representation in Figure 12 provides a comprehensive overview of the complex web of international collaborations, underscoring the pivotal role of the United States as a central hub and the diverse range of global partnerships that shape the dynamics of this research field.
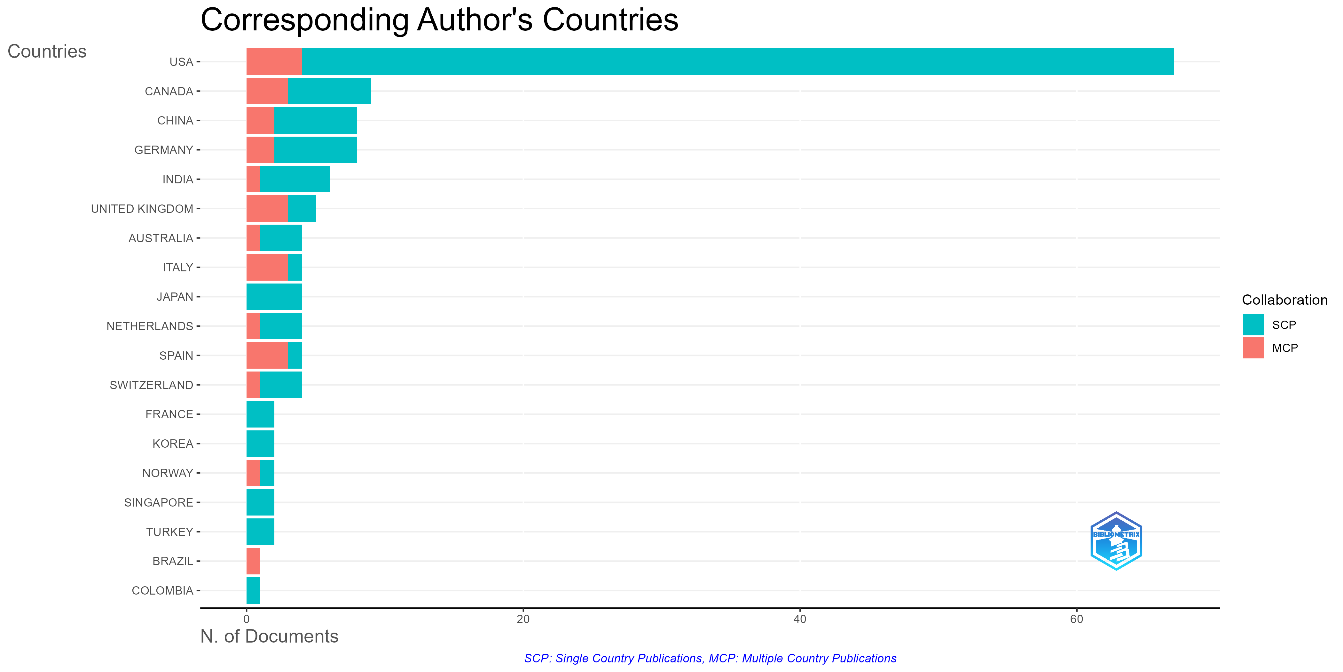
Figure 12. Corresponding Author's Countries
This observation is further supported by the findings from Figure 10, which analyzes international collaboration in research publications. The data reveals that the United States is the dominant contributor, with a significant presence in single-country and multiple-country publications, cementing its central role in this field.
However, the picture is far from one-sided. Substantial international collaboration is evident, with countries like Canada, China, Germany, the United Kingdom, and Italy engaging in notable cross-border partnerships. This collaborative spirit reflects the inherently global nature of the research topic.
Interestingly, a new generation of players is also making its mark. Emerging contributors such as India, Switzerland, Spain, Singapore, and South Korea enrich the global landscape, indicating a growing interest and involvement in this domain. The varying ratios of single-country to multiple-country publications across these nations suggest differing collaboration intensities, with Italy and Spain demonstrating a solid focus on joint research efforts.
Furthermore, the geographic distribution of research activity points to regional hubs in North America, Europe, and Asia, where the concentration of work is more pronounced. This spatial pattern highlights the interconnected nature of the scientific community, with established powerhouses and newcomers working together to drive progress in this field.
Overall, this landscape tells a story of a dynamic interplay between dominant players and emerging voices, underscoring the collaborative nature of advancements in this scientific domain. The data and network visualization paint a picture of an increasingly global and interconnected research landscape, fostering the exchange of ideas and the progression of knowledge across borders.
Research Themes and Emerging Topics
Core Themes in XAI and ACP
Figure 13 presents a conceptual framework that maps various themes related to Explainable AI (XAI) and Advance Care Planning (ACP) based on their "Relevance degree (Centrality)" and "Development degree (Density)." In the "Niche Themes" region of the framework, topics like "cancer survival," "overall survival," and "pathology" are depicted. These themes have a lower degree of relevance but a higher degree of development, suggesting they are specialized or niche topics within the broader context of XAI and ACP research. The "Motor Themes" region is currently empty, indicating that there are no dominant themes that are highly relevant and developed at this point. The "Emerging or Declining Themes" region includes topics such as "artificial intelligence," "advance care planning," and "terminal care." These themes have a lower development degree but a higher relevance degree, signaling that they are emerging or gaining importance in the fields of XAI and ACP. The "Basic Themes" region is also empty, meaning there are no fundamental or basic themes that are both low relevant and low developed at this stage. The placement of the terms "human," article," and "humans" within the framework suggests that they may contextualize or differentiate the themes presented. Lastly, Figure 15 visually represents the thematic landscape, highlighting the relative importance and maturity of various topics within the intersection of XAI and ACP research.
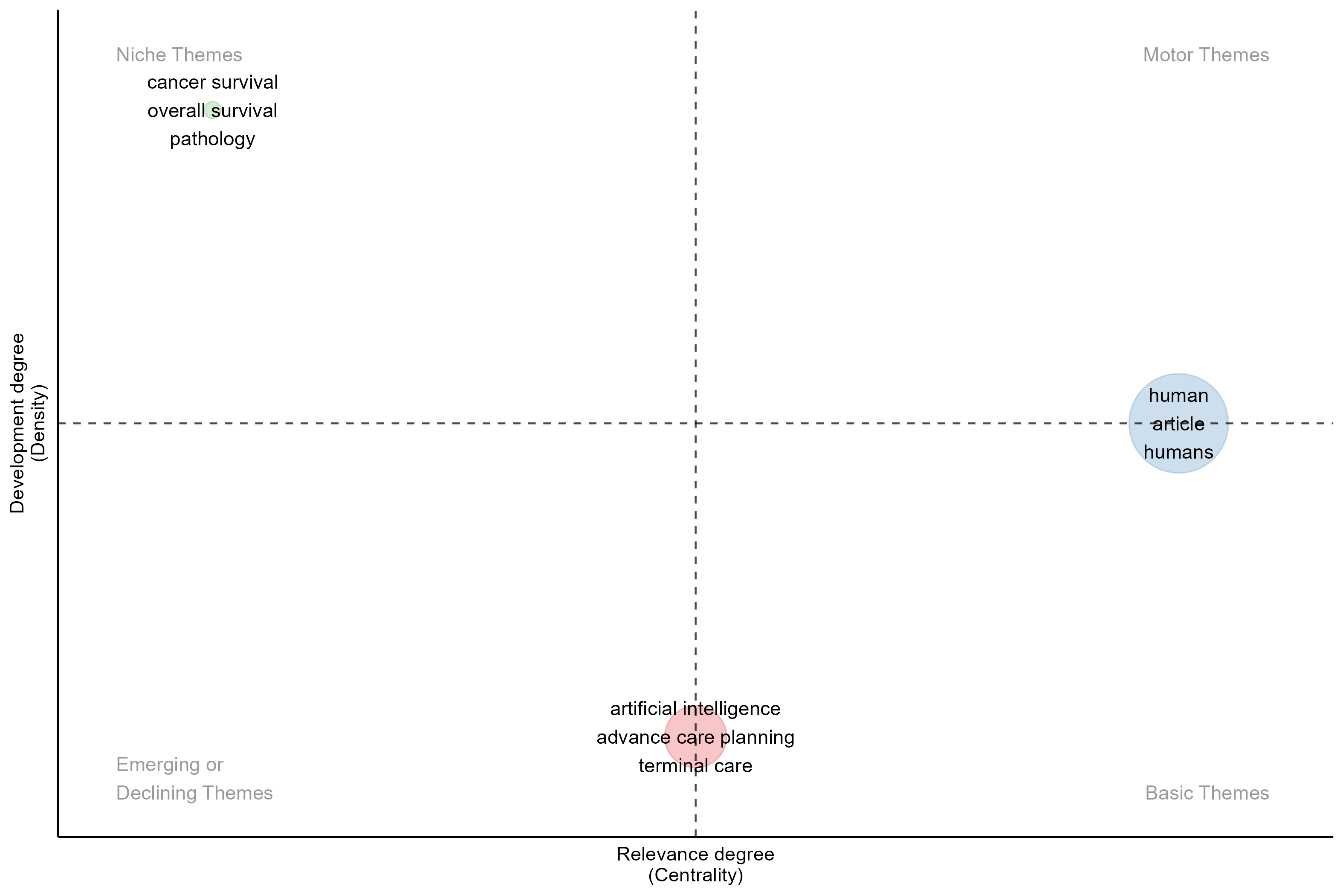
Figure 13. Thematic Map
Emerging Topic and Trendy Keywords
The analysis of recent publications reveals significant emerging topics and trendy keywords within Explainable AI (XAI) and Advance Care Planning (ACP). In Table 20 present, A standout term is "machine learning," which has a frequency of 159 occurrences, marking its increasing prominence in the literature since 2021. This reflects a broader trend in healthcare research, where machine learning techniques are widely adopted for various applications, including predictive modeling and decision-making. Additionally, key emerging topics include "human" (142 occurrences) and "humans" (120 occurrences), which highlight the importance of understanding user needs and experiences in the context of XAI and ACP. The analysis also identifies significant themes such as "mortality" (32 occurrences) and "hospitalization" (50 occurrences), underscoring critical areas of concern within healthcare. The term "electronic health record," appearing 20 times, indicates the ongoing integration of technology in patient care, while topics related to specific demographics, such as "young adult" (17 occurrences) and "length of stay" (12 occurrences), emphasize the need for tailored approaches in advance care planning can be seen in Table 7.
Table 7. Trend Topics
Item | Freq | Year_q1 | Year_med | Year_q3 |
machine learning | 159 | 2021 | 2022 | 2023 |
human | 142 | 2021 | 2022 | 2024 |
article | 121 | 2021 | 2023 | 2024 |
humans | 120 | 2021 | 2022 | 2023 |
hospitalization | 50 | 2022 | 2023 | 2023 |
artificial intelligence | 49 | 2023 | 2023 | 2024 |
mortality | 32 | 2020 | 2021 | 2023 |
electronic health record | 20 | 2020 | 2021 | 2022 |
young adult | 17 | 2020 | 2021 | 2023 |
length of stay | 12 | 2023 | 2024 | 2024 |
intensive care unit | 10 | 2022 | 2024 | 2024 |
health care personnel | 8 | 2020 | 2020 | 2024 |
infant | 8 | 2022 | 2024 | 2024 |
priority journal | 7 | 2020 | 2020 | 2021 |
epidemiology | 6 | 2019 | 2020 | 2022 |
documentation | 5 | 2019 | 2019 | 2024 |
medicare | 5 | 2019 | 2019 | 2021 |
The keyword analysis of the literature surrounding Explainable AI (XAI) and Advance Care Planning (ACP) reveal several significant trends and focus areas within this interdisciplinary field. The word cloud data in Figure 6 provides valuable insights into the primary themes and their relative importance in current research.
Machine learning emerges as the most prominent term, with a frequency of 159 occurrences, underscoring its central role in developing XAI applications for ACP. This prevalence indicates a strong emphasis on leveraging advanced computational methods to enhance decision-making processes in healthcare, particularly in complex scenarios such as end-of-life care [70]. The high frequency of human-related terms, including "human" (142 occurrences), "humans" (120 occurrences), and demographic indicators like "female" (113 occurrences) and "male" (109 occurrences), highlights the critical importance of human factors and demographic considerations in the implementation of XAI systems [71]. This focus aligns with recent research emphasizing the need for AI technologies that are not only technically proficient but also socially responsible and equitable, addressing potential biases and health disparities [72].
The significant presence of terms related to palliative care, such as "palliative therapy" (101 occurrences) and "palliative care" (67 occurrences), indicates a specific interest in applying XAI within end-of-life care scenarios. This trend reflects the growing recognition of AI's potential to improve diagnostic accuracy and decision-making in complex clinical settings, with some studies suggesting improvements of up to 30% in decision accuracy [73]. The emphasis on palliative care also underscores the ethical challenges and considerations inherent in implementing AI technologies in sensitive healthcare domains, including concerns about patient data privacy and the potential for dehumanization of care.

Figure 14. Word Cloud for Most frequent words
Age-related terms like "adult" (98 occurrences) and "aged" (76 occurrences) further emphasize the relevance of XAI and ACP to older populations, who often face unique challenges in healthcare decision-making. This demographic focus aligns with the need for personalized care and decision support systems to analyze large datasets to identify patterns and trends, potentially leading to more effective symptom management and improved patient outcomes [73].
This analysis of emerging topics and keywords illustrates a dynamic landscape in XAI and ACP research, characterized by a strong emphasis on machine learning, human-centered approaches, and the integration of technology to address pressing healthcare challenges.
Thematic Cluster
The thematic mapping of the research landscape for Explainable AI (XAI) in Advance Care Planning (ACP) highlights three key focus clusters. The first cluster centers around "human" factors, with a significant Callon centrality score of 56.30 and a density of 91.72. This cluster reflects the critical importance of understanding user needs and experiences in implementing XAI systems, emphasizing a shift towards human-centered approaches in AI research.
The second cluster focuses on "artificial intelligence," with a Callon centrality score of 25.97 and a density of 71.25. This indicates a growing interest in leveraging AI technologies to enhance decision-making processes and improve patient outcomes in healthcare contexts. The emphasis on artificial intelligence highlights its central role in developing XAI applications for ACP.
Lastly, the third cluster addresses "cancer survival," which has a lower Callon centrality score of 9.27 but a high density of 95.33. This cluster indicates a specific interest in applying XAI to improve cancer patients' outcomes, showcasing the potential of AI technologies to assist in complex clinical decision-making.
Together, these thematic clusters underscore the multifaceted nature of XAI in ACP, illustrating the interplay between advanced technology, human factors, and specific health conditions in shaping future research directions can be seen in Table 8.
Table 8. Thematic Cluster
Cluster | Callon Centrality | Callon Density | Rank Centrality | Rank Density | Cluster Frequency |
human | 56.30475531418639 | 91.71864602735461 | 3 | 2 | 2187 |
artificial intelligence | 25.96528123578161 | 71.24684279869483 | 2 | 1 | 551 |
cancer survival | 9.26773629148629 | 95.33087015798056 | 1 | 3 | 106 |
Temporal Evolution of Topics
The evolution of research topics from 2019 to 2024 (see Figure 15) illustrates a clear transition in focus areas:
- 2019–2023: The initial research phase primarily concentrated on palliative therapy, prognosis, and human factors. Key topics included the development of palliative care strategies, understanding patient prognosis, and integrating human-centered approaches in healthcare. This period emphasized foundational concepts related to patient care, algorithmic approaches to prognosis, and the importance of human factors in healthcare decision-making.
- 2024: The latter phase significantly shifts towards more specific applications and methodologies. This period saw the emergence of topics such as decision-making, mortality, and advance care planning, reflecting a deeper engagement with the complexities of patient care in real-world settings. Additionally, the introduction of randomized controlled trials signifies a strong emphasis on empirical evaluation of XAI tools. The focus on accuracy highlights the ongoing quest for reliable AI applications in healthcare. Other key themes included consultation processes and using artificial intelligence chatbots to enhance patient interactions. Finally, content analysis emerged as a vital method for understanding the effectiveness and implications of these technologies in healthcare settings.
This evolution showcases a transition from foundational research to practical applications, emphasizing the integration of AI tools in enhancing decision-making processes and improving patient outcomes in healthcare.
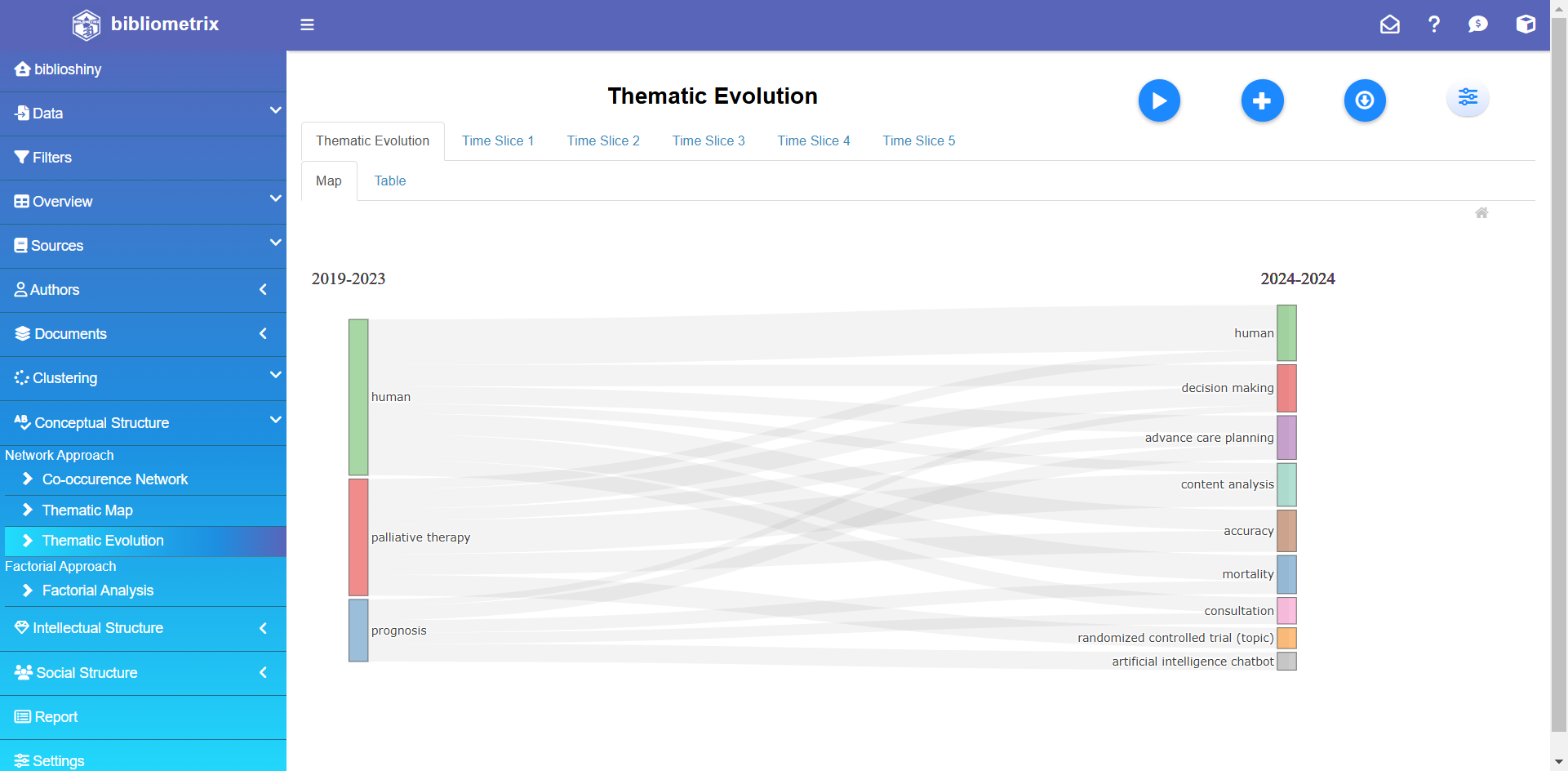
Figure 15. Thematic Evolution
Keyword Co-Occurrence Networks
The co-occurrence network analysis (see Figure 16) reveals significant insights into the interconnections among various research topics related to Explainable AI (XAI) and Advance Care Planning (ACP). Artificial intelligence emerges as a crucial focal point, reflecting its central role in the network. Related topics, such as qualitative research and natural language processing, enhance the understanding of AI applications in healthcare, albeit with varying levels of influence.
Furthermore, decision-making and hospice care are vital themes, indicating their relevance in discussions about patient care. The nodes for clinical articles and conversations suggest a strong emphasis on communication and documentation within healthcare settings. The analysis also highlights a focus on empirical research methodologies, with terms like major clinical studies and hospitalization showcasing their importance in assessing patient outcomes and healthcare delivery.
In another cluster, terms related to machine learning and human factors demonstrate the integration of advanced analytics with human-centered approaches in healthcare research. This includes discussions on palliative therapy and prognosis, emphasizing the importance of understanding patient needs and treatment effectiveness.
The presence of themes such as mortality, quality of life, and terminal care indicates ongoing research focused on critical aspects of patient care, particularly for vulnerable populations like the elderly and cancer patients. Innovative approaches, such as artificial intelligence chatbots and content analysis, reflect efforts to enhance patient interaction and evaluate the effectiveness of XAI tools.
The co-occurrence network illustrates a complex web of relationships among various research topics. This interconnectedness highlights the multifaceted nature of XAI and its applications in improving patient care and outcomes in healthcare settings, emphasizing the need for an integrated approach that combines technological advancements with a deep understanding of human factors and clinical practices.
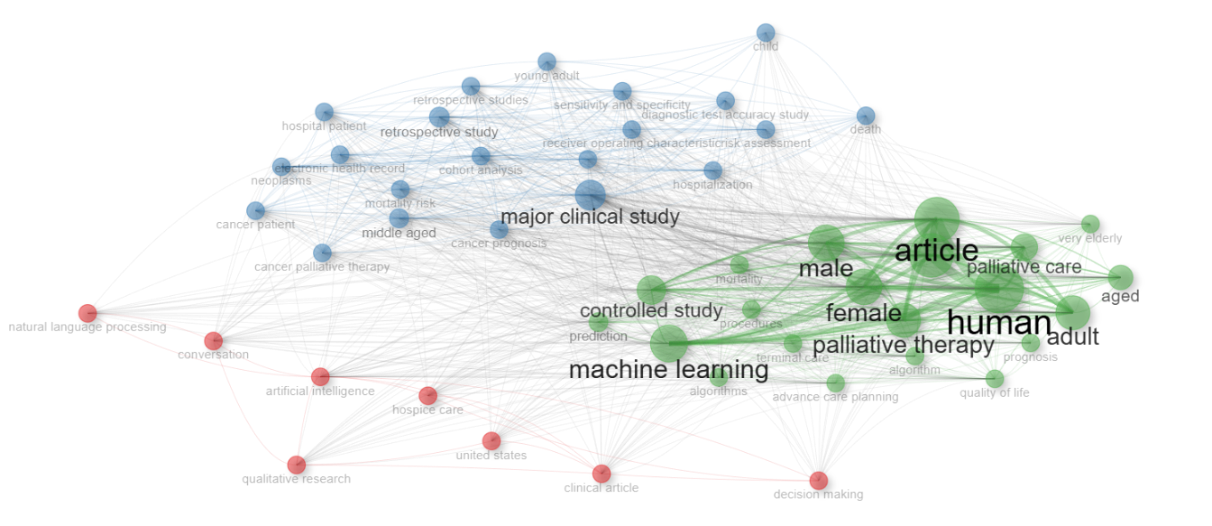
Figure 16. Co-occurrence Network
CONCLUSIONS
The bibliometric analysis of Explainable AI (XAI) in Advance Care Planning (ACP) from 2019 to 2024 reveals a dynamic and rapidly evolving research landscape. This study encompasses 160 documents from 101 distinct publications, demonstrating a robust annual growth rate of 44.43%. The dataset reflects the significant impact of these recent publications, with an average age of 1.71 years and an average of 7.025 citations per document. A comprehensive keywords analysis highlights a rich diversity of themes, with 1,489 Keywords Plus and 523 Author's Keywords, underscoring critical trends in the field. The authorship landscape is notably collaborative, involving 1,024 authors with an average of 7.57 co-authors per document and 18.75% of the documents resulting from international collaborations. All analyzed documents are peer-reviewed research articles, ensuring a rigorous approach to relevant research questions. The University of Pennsylvania is a leading contributor with 85 publications, followed by Stanford University School of Medicine and the University of Vermont.
The United States dominates geographically with 673 publications, while Germany, China, and Canada contribute significantly. Prominent authors, such as Dr. RB Parikh and Dr. C Chivers, exemplify substantial contributions, showcasing the collaborative nature of XAI and ACP research. Key journals, particularly the *Journal of Pain and Symptom Management* and the *Journal of Palliative Medicine*, have significantly advanced the literature on XAI in ACP. The bibliometric data indicates a marked increase in publication output, especially post-2021, reflecting a growing recognition of the importance of integrating XAI into healthcare practices. These journals are pivotal in enhancing patient-centered care and informing clinical decision-making, indicating they will remain central to the discourse on XAI in ACP. The analysis of collaboration networks reveals distinct clusters of researchers, highlighting the role of institutions like Harvard Medical School as pivotal centers for collaboration. The United States serves as a dominant hub, with increasing contributions from emerging countries such as India and Singapore, fostering a vibrant global landscape for research. The thematic analysis identifies critical areas of focus, including niche themes like "cancer survival" and emerging topics such as "artificial intelligence" and "advance care planning." The prominence of "machine learning" reflects its significant role in healthcare applications, while human-centered approaches emphasize the importance of user experiences. The temporal evolution of topics indicates a shift from foundational research to practical applications, particularly in decision-making and mortality. The integration of XAI into ACP practices has important implications. XAI tools can enhance communication between patients and healthcare providers, ensuring that patient values and preferences are accurately reflected in care decisions, leading to more personalized treatment plans. By providing clear explanations for AI-generated recommendations, XAI empowers patients and families to make informed choices about their care options, fostering greater autonomy. However, healthcare professionals must receive training to effectively utilize XAI tools, highlighting the necessity for interdisciplinary collaboration. Policymakers are also encouraged to develop frameworks that facilitate the adoption of XAI in healthcare settings, addressing ethical considerations and promoting transparency to build trust among patients and providers. Several vital areas require attention to enhance the integration of XAI in ACP. There is a pressing need for user-friendly XAI tools that can be easily incorporated into healthcare systems to improve usability for both providers and patients. Establishing ethical guidelines for using XAI in ACP is crucial, particularly concerning patient privacy and autonomy. Additionally, investigating the real-world implementation of XAI across various healthcare settings will help assess its effectiveness and identify potential barriers to adoption. Longitudinal studies examining the long-term impacts of XAI on ACP outcomes and patient satisfaction will yield valuable insights into the sustainability of these technologies.
Ultimately, fostering interdisciplinary collaboration among AI researchers, healthcare professionals, ethicists, and policymakers will be essential to tackle the multifaceted challenges of implementing XAI in ACP. Addressing these implications and pursuing future research directions has significant potential to improve healthcare outcomes and honor patient preferences in critical care decisions.
REFERENCES
- WHO, ‘Ageing and health’. Accessed: Oct. 23, 2024. https://www.who.int/news-room/fact-sheets/detail/ageing-and-health.
- A. Balachandran, “Population ageing in Europe and Asia: Beyond traditional perspectives,” University of Groningen, 2020, https://doi.org/10.33612/diss.135497884.
- G. Shackman, X. Wang, and Y.-L. Liu, “Brief Review of World Demographic Trends - Trends in Age Distributions,” SSRN Electron. J., 2012, https://doi.org/10.2139/ssrn.2180600.
- B. C. Vladeck and J. P. Firman, “The Aging of the Population and Health Services,” Ann. Am. Acad. Pol. Soc. Sci., vol. 468, no. 1, pp. 132–148, 1983, https://doi.org/10.1177/0002716283468001009.
- F. T. Denton and B. G. Spencer, “Chronic Health Conditions: Changing Prevalence in an Aging Population and Some Implications for the Delivery of Health Care Services,” Can. J. Aging Rev. Can. Vieil., vol. 29, no. 1, pp. 11–21, 2010, https://doi.org/10.1017/S0714980809990390.
- T. M. Dall, P. D. Gallo, R. Chakrabarti, T. West, A. P. Semilla, and M. V. Storm, “An Aging Population And Growing Disease Burden Will Require ALarge And Specialized Health Care Workforce By 2025,” Health Aff. (Millwood), vol. 32, no. 11, pp. 2013–2020, 2013, https://doi.org/10.1377/hlthaff.2013.0714.
- T. R. Fried, E. H. Bradley, V. R. Towle, and H. Allore, “Understanding the Treatment Preferences of Seriously Ill Patients,” N. Engl. J. Med., vol. 346, no. 14, pp. 1061–1066, 2002, https://doi.org/10.1056/NEJMsa012528.
- J. S. Weiner and S. A. Cole, “Three Principles to Improve Clinician Communication for Advance Care Planning: Overcoming Emotional, Cognitive, and Skill Barriers,” J. Palliat. Med., vol. 7, no. 6, pp. 817–829, 2004, https://doi.org/10.1089/jpm.2004.7.817.
- M.-K. Song et al., “Effects of an intervention to improve communication about end-of-life care among African Americans with chronic kidney disease,” Appl. Nurs. Res., vol. 23, no. 2, pp. 65–72, 2010, https://doi.org/10.1016/j.apnr.2008.05.002.
- J. L. Holley and J. A. Yasunaga, “Advance Care Planning to Elicit and Respect Patient Values and Preferences,” in Palliative Care in Nephrology, pp. 98–107, 2020, https://doi.org/10.1093/med/9780190945527.003.0010.
- W. E. Rosa et al., “Advance Care Planning in Serious Illness: A Narrative Review,” J. Pain Symptom Manage., vol. 65, no. 1, pp. e63–e78, 2023, https://doi.org/10.1016/j.jpainsymman.2022.08.012.
- R. C. Kolarik, R. M. Arnold, G. S. Fischer, and J. A. Tulsky, “Objectives for Advance Care Planning,” J. Palliat. Med., vol. 5, no. 5, pp. 697–704, 2002, https://doi.org/10.1089/109662102320880516.
- C. Sedini, M. Biotto, L. M. Crespi Bel’skij, R. E. Moroni Grandini, and M. Cesari, “Advance care planning and advance directives: an overview of the main critical issues,” Aging Clin. Exp. Res., vol. 34, no. 2, pp. 325–330, 2022, https://doi.org/10.1007/s40520-021-02001-y.
- M. Butler, E. Ratner, E. McCreedy, N. Shippee, and R. L. Kane, “Decision Aids for Advance Care Planning: An Overview of the State of the Science”, Ann. Intern. Med., vol. 161, no. 6, p. 408, 2014, https://doi.org/10.7326/M14-0644.
- C. E. Low et al., “A cross-sectional study on advance care planning documentation attitudes during national advance care planning week in a South-East Asian country,” BMC Palliat. Care, vol. 23, no. 1, p. 244, 2024, https://doi.org/10.1186/s12904-024-01505-4.
- C. Burris and D. Sevier, “Sidebar: Enhancing Technology to Better Communicate Advance Care Planning Information,” N. C. Med. J., vol. 81, no. 4, pp. 245–246, 2020, https://doi.org/10.18043/ncm.81.4.245.
- M. J. Green and B. H. Levi, ‘The era of “e”: The use of new technologies in advance care planning’, Nurs. Outlook, vol. 60, no. 6, pp. 376-383.e2, 2012, https://doi.org/10.1016/j.outlook.2012.08.005.
- S. Bose-Brill and T. R. Pressler, “Commentary: Opportunities for Innovation and Improvement in Advance Care Planning Using a Tethered Patient Portal in the Electronic Health Record,” J. Prim. Care Community Health, vol. 3, no. 4, pp. 285–288, 2012, https://doi.org/10.1177/2150131911435525.
- J. Kraft, “Injecting social technology into advance care planning,” BMJ Support. Palliat. Care, vol. 2, no. 2, p. 199.2-199, 2012, https://doi.org/10.1136/bmjspcare-2012-000250.107.
- T. Davenport and R. Kalakota, “The potential for artificial intelligence in healthcare,” Future Healthc. J., vol. 6, no. 2, pp. 94–98, 2019, https://doi.org/10.7861/futurehosp.6-2-94.
- L. De Panfilis, C. Peruselli, S. Tanzi, and C. Botrugno, “AI-based clinical decision-making systems in palliative medicine: ethical challenges,” BMJ Support. Palliat. Care, vol. 13, no. 2, pp. 183–189, 2023, https://doi.org/10.1136/bmjspcare-2021-002948.
- D. C. McElfresh et al., “Can an Algorithm Be My Healthcare Proxy?,” in Explainable AI in Healthcare and Medicine, vol. 914, pp. 313–319, 2021, https://doi.org/10.1007/978-3-030-53352-6_30.
- C. Giordano, M. Brennan, B. Mohamed, P. Rashidi, F. Modave, and P. Tighe, “Accessing Artificial Intelligence for Clinical Decision-Making,” Front. Digit. Health, vol. 3, p. 645232, 2021, https://doi.org/10.3389/fdgth.2021.645232.
- G. Cano-Verdugo, J. Owoyemi, A. Khan, M. Sadman Tahsin, N. Jiwani, and D. N. Shukurullaevna, “Leveraging Artificial Intelligence to Revolutionize Healthcare: A Comprehensive Analysis,” SciWaveBulletin, vol. 01, no. 01, pp. 12–19, 2023, https://doi.org/10.61925/SWB.2023.1103.
- M. Ghassemi, L. Oakden-Rayner, and A. L. Beam, “The false hope of current approaches to explainable artificial intelligence in health care,” Lancet Digit. Health, vol. 3, no. 11, pp. e745–e750, 2021, https://doi.org/10.1016/S2589-7500(21)00208-9.
- A. F. Markus, J. A. Kors, and P. R. Rijnbeek, “The role of explainability in creating trustworthy artificial intelligence for health care: A comprehensive survey of the terminology, design choices, and evaluation strategies,” J. Biomed. Inform., vol. 113, p. 103655, 2021, https://doi.org/10.1016/j.jbi.2020.103655.
- N. Bienefeld et al., “Solving the explainable AI conundrum by bridging clinicians’ needs and developers’ goals,” Npj Digit. Med., vol. 6, no. 1, p. 94, 2023, https://doi.org/10.1038/s41746-023-00837-4.
- C. C. Yang, “Explainable Artificial Intelligence for Predictive Modeling in Healthcare,” J. Healthc. Inform. Res., vol. 6, no. 2, pp. 228–239, 2022, https://doi.org/10.1007/s41666-022-00114-1.
- N. Rane, S. Choudhary, and J. Rane, “Explainable Artificial Intelligence (XAI) in healthcare: Interpretable Models for Clinical Decision Support,” SSRN Electron. J., 2023, https://doi.org/10.2139/ssrn.4637897.
- R. Mariappan, “Extensive Review of Literature on Explainable AI (XAI) in HealthcareApplications’, Recent Adv. Comput. Sci. Commun., vol. 17, 2024, https://doi.org/10.2174/0126662558296699240314055348.
- Z. Sadeghi et al., “A brief review of explainable artificial intelligence in healthcare,” arXiv preprint arXiv:2304.01543, 2023, https://doi.org/10.48550/arXiv.2304.01543.
- T. Hulsen, “Explainable Artificial Intelligence (XAI): Concepts and Challenges in Healthcare,” AI, vol. 4, no. 3, pp. 652–666, 2023, https://doi.org/10.3390/ai4030034.
- U. B. Khakurel and D. B. Rawat, “Evaluating explainable artificial intelligence (XAI): algorithmic explanations for transparency and trustworthiness of ML algorithms and AI systems,” in Artificial Intelligence and Machine Learning for Multi-Domain Operations Applications IV, p. 7, 2022, https://doi.org/10.1117/12.2620598.
- N. Thalpage, “Unlocking the Black Box: Explainable Artificial Intelligence (XAI) for Trust and Transparency in AI Systems,” J. Digit. Art Humanit., vol. 4, no. 1, pp. 31–36, 2023, https://doi.org/10.33847/2712-8148.4.1_4.
- R. Tiwari, “Explainable AI (XAI) and its Applications in Building Trust and Understanding in AI Decision Making,” INTERANTIONAL J. Sci. Res. Eng. Manag., vol. 07, no. 01, 2023, https://doi.org/10.55041/IJSREM17592.
- R. S. Deshpande, P. V. Ambatkar, “Interpretable Deep Learning Models: Enhancing Transparency and Trustworthiness in Explainable AI,” Proceeding Int. Conf. Sci. Eng., vol. 11, no. 1, pp. 1352–1363, 2023, https://doi.org/10.52783/cienceng.v11i1.286.
- Q. Xu et al., “Interpretability of Clinical Decision Support Systems Based on Artificial Intelligence from Technological and Medical Perspective: A Systematic Review,” J. Healthc. Eng., vol. 2023, no. 1, p. 9919269, 2023, https://doi.org/10.1155/2023/9919269.
- T. Sethi, A. Kalia, A. Sharma, and A. Nagori, “Interpretable artificial intelligence: Closing the adoption gap in healthcare,” in Artificial Intelligence in Precision Health, pp. 3–29, 2020, https://doi.org/10.1016/B978-0-12-817133-2.00001-X.
- A. Duenser and D. M. Douglas, “Whom to Trust, How and Why: Untangling Artificial Intelligence Ethics Principles, Trustworthiness, and Trust,” IEEE Intell. Syst., vol. 38, no. 6, pp. 19–26, 2023, https://doi.org/10.1109/MIS.2023.3322586.
- J. Zhang and Z. Zhang, “Ethics and governance of trustworthy medical artificial intelligence,” BMC Med. Inform. Decis. Mak., vol. 23, no. 1, p. 7, 2023, https://doi.org/10.1186/s12911-023-02103-9.
- R. Dlugatch, A. Georgieva, and A. Kerasidou, “Trustworthy artificial intelligence and ethical design: public perceptions of trustworthiness of an AI-based decision-support tool in the context of intrapartum care,” BMC Med. Ethics, vol. 24, no. 1, p. 42, 2023, https://doi.org/10.1186/s12910-023-00917-w.
- C. González-Gonzalo et al., “Trustworthy AI: Closing the gap between development and integration of AI systems in ophthalmic practice,” Prog. Retin. Eye Res., vol. 90, p. 101034, 2022, https://doi.org/10.1016/j.preteyeres.2021.101034.
- H. D. Lum, R. L. Sudore, and D. B. Bekelman, “Advance Care Planning in the Elderly,” Med. Clin. North Am., vol. 99, no. 2, pp. 391–403, 2015, https://doi.org/10.1016/j.mcna.2014.11.010.
- L. E. Dingfield and J. B. Kayser, “Integrating Advance Care Planning Into Practice,” Chest, vol. 151, no. 6, pp. 1387–1393, 2017, https://doi.org/10.1016/j.chest.2017.02.024.
- N. Pease, “Advance care-planning and clinical decision-making,” Medicine (Baltimore), vol. 48, no. 1, pp. 57–60, 2020, https://doi.org/10.1016/j.mpmed.2019.10.012.
- S. S. Sullivan, “TakingAIM: A Precision Health Framework for Promoting Person-Centered Advance Care Planning,” J. Hosp. Palliat. Nurs., vol. 21, no. 6, pp. 502–509, 2019, https://doi.org/10.1097/NJH.0000000000000560.
- A. Choudhury, “Toward an Ecologically Valid Conceptual Framework for the Use of Artificial Intelligence in Clinical Settings: Need for Systems Thinking, Accountability, Decision-making, Trust, and Patient Safety Considerations in Safeguarding the Technology and Clinicians,” JMIR Hum. Factors, vol. 9, no. 2, p. e35421, 2022, https://doi.org/10.2196/35421.
- I. Passas, “Bibliometric Analysis: The Main Steps,” Encyclopedia, vol. 4, no. 2, pp. 1014–1025, 2024, https://doi.org/10.3390/encyclopedia4020065.
- D. F. Thompson and C. K. Walker, “A Descriptive and Historical Review of Bibliometrics with Applications to Medical Sciences,” Pharmacother. J. Hum. Pharmacol. Drug Ther., vol. 35, no. 6, pp. 551–559, 2015, https://doi.org/10.1002/phar.1586.
- M. D. S. T. Silva, V. M. D. Oliveira, and S. É. N. Correia, “Scientific mapping in Scopus with Biblioshiny: A bibliometric analysis of organizational tensions,” Context. – Rev. Contemp. Econ. E Gest., vol. 20, pp. 54–71, 2022, https://doi.org/10.19094/contextus.2022.72151.
- H. K. Kondaveeti, S. Raman, and P. Raj, “Prototyping with Raspberry Pi in Healthcare Domain,” Int. J. Adv. Comput. Sci. Appl., vol. 11, no. 10, 2020, https://doi.org/10.14569/IJACSA.2020.0111038.
- M. N. Akhtar, A. Haleem, and M. Javaid, “Exploring the advent of Medical 4.0: A bibliometric analysis systematic review and technology adoption insights,” Inform. Health, vol. 1, no. 1, pp. 16–28, 2024, https://doi.org/10.1016/j.infoh.2023.10.001.
- A. A. Olariu, A. Breazu, Ștefan C. Popa, C. F. Popa, and N. Căruceru, “Decision-Making in Healthcare. A Bibliometric Exploration,” Proc. Int. Conf. Bus. Excell., vol. 18, no. 1, pp. 3242–3254, 2024, https://doi.org/10.2478/picbe-2024-0264.
- E. M. Kenny, E. D. Delaney, D. Greene, and M. T. Keane, “Post-hoc Explanation Options for XAI in Deep Learning: The Insight Centre for Data Analytics Perspective,” in Pattern Recognition. ICPR International Workshops and Challenges, vol. 12663, pp. 20–34, 2021, https://doi.org/10.1007/978-3-030-68796-0_2.
- G. Yang, Q. Ye, and J. Xia, “Unbox the black-box for the medical explainable AI via multi-modal and multi-centre data fusion: A mini-review, two showcases and beyond,” Inf. Fusion, vol. 77, pp. 29–52, 2022, https://doi.org/10.1016/j.inffus.2021.07.016.
- D. Wang, Q. Yang, A. Abdul, and B. Y. Lim, “Designing Theory-Driven User-Centric Explainable AI,” in Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems, , pp. 1–15, 2019, https://doi.org/10.1145/3290605.3300831.
- B. L. Kass-Bartelmes and R. Hughes, “Advance Care Planning: Preferences for Care at the End of Life,” J. Pain Palliat. Care Pharmacother., vol. 18, no. 1, pp. 87–109, 2004, https://doi.org/10.1080/J354v18n01_08.
- A. U. Patel, Q. Gu, R. Esper, D. Maeser, and N. Maeser, “The Crucial Role of Interdisciplinary Conferences in Advancing Explainable AI in Healthcare,” BioMedInformatics, vol. 4, no. 2, pp. 1363–1383, 2024, https://doi.org/10.3390/biomedinformatics4020075.
- S. Ali, A. S. Imran, Z. Kastrati, and S. M. Daudpota, “Visualizing Research on Explainable Artificial Intelligence for Medical and Healthcare,” in 2023 4th International Conference on Computing, Mathematics and Engineering Technologies (iCoMET), pp. 1–6, 2023, https://doi.org/10.1109/iCoMET57998.2023.10099343.
- C.-J. Liu et al., “A Worldwide Bibliometric Analysis of Publications on Advance Care Planning in the Past 3 Decades,” Am. J. Hosp. Palliat. Med., vol. 37, no. 6, pp. 474–480, 2020, https://doi.org/10.1177/1049909119886305.
- Y. Lai, A. Kankanhalli, and D. Ong, “Human-AI Collaboration in Healthcare: A Review and Research Agenda,” presented at the Hawaii International Conference on System Sciences, 2021, https://doi.org/10.24251/HICSS.2021.046.
- J. Baas, M. Schotten, A. Plume, G. Côté, and R. Karimi, “Scopus as a curated, high-quality bibliometric data source for academic research in quantitative science studies,” Quant. Sci. Stud., vol. 1, no. 1, pp. 377–386, 2020, https://doi.org/10.1162/qss_a_00019.
- B. L. Jimma, “Artificial intelligence in healthcare: A bibliometric analysis,” Telemat. Inform. Rep., vol. 9, p. 100041, 2023, https://doi.org/10.1016/j.teler.2023.100041.
- M. Schotten, M. El Aisati, W. J. N. Meester, S. Steiginga, and C. A. Ross, “A Brief History of Scopus: The World’s Largest Abstract and Citation Database of Scientific Literature,” in Research Analytics, pp. 31–58, 2017, https://doi.org/10.1201/9781315155890-3.
- M. Visser, N. J. Van Eck, and L. Waltman, “Large-scale comparison of bibliographic data sources: Scopus, Web of Science, Dimensions, Crossref, and Microsoft Academic,” Quant. Sci. Stud., vol. 2, no. 1, pp. 20–41, 2021, https://doi.org/10.1162/qss_a_00112.
- V. Devaki, Dr. E. Ramganesh, and Dr. S. Amutha, “Bibliometric Analysis on Metacognition and Self-Regulation Using Biblioshiny Software,” Indian J. Inf. Sources Serv., vol. 14, no. 2, pp. 115–125, 2024, https://doi.org/10.51983/ijiss-2024.14.2.17 .
- J. Ali, A. Jusoh, N. Idris, A. G. Airij, and R. Chandio, “Wearable Devices in Healthcare Services. Bibliometrix Analysis by using R Package,” Int. J. Online Biomed. Eng. IJOE, vol. 18, no. 08, pp. 61–86, 2022, https://doi.org/10.3991/ijoe.v18i08.31785.
- C. R. Manz et al., “Validation of a Machine Learning Algorithm to Predict 180-Day Mortality for Outpatients With Cancer,” JAMA Oncol., vol. 6, no. 11, p. 1723, 2020, https://doi.org/10.1001/jamaoncol.2020.4331.
- K. Jung et al., “A framework for making predictive models useful in practice,” J. Am. Med. Inform. Assoc., vol. 28, no. 6, pp. 1149–1158, 2021, https://doi.org/10.1093/jamia/ocaa318.
- E. Vu et al., “Applications of Machine Learning in Palliative Care: A Systematic Review,” Cancers, vol. 15, no. 5, p. 1596, 2023, https://doi.org/10.3390/cancers15051596.
- M. Knop, S. Weber, M. Mueller, and B. Niehaves, “Human Factors and Technological Characteristics Influencing the Interaction of Medical Professionals With Artificial Intelligence–Enabled Clinical Decision Support Systems: Literature Review,” JMIR Hum. Factors, vol. 9, no. 1, p. e28639, 2022, https://doi.org/10.2196/28639.
- I. Dankwa-Mullan, “Health Equity and Ethical Considerations in Using Artificial Intelligence in Public Health and Medicine,” Prev. Chronic. Dis., vol. 21, p. 240245, 2024, https://doi.org/10.5888/pcd21.240245.
- U. Munive Jesus, “Incorporating artificial intelligence in palliative care: opportunities and challenges,” Hosp. Palliat. Med. Int. J., vol. 7, no. 3, pp. 81–83, 2024, https://doi.org/10.15406/hpmij.2024.07.00244.
AUTHOR BIOGRAPHY

| Irianna Futri received her bachelor’s degree in information systems from the Nurdin Hamzah School of Computer and Informatics Management in Jambi, Indonesia, in 2011. She worked at The Construction Services Public Works Department Jambi for 1 year as an Administrator for SIPJAKI (Construction Services Development Information System). She also worked as an informatics teacher at the Vocational School of Dharma Bhakti 4 for 3 years and served as an Operator for Dapodik for 7 years. She is pursuing a master’s degree in international technology and Innovation Management at the International College, Khon Kaen University, Khon Kaen, Thailand. Her current research interests include advanced care plans and bibliometric analysis. Email: irianna.f@kkumail.com, Orcid: 0009-0003-7100-3583. |
|
|

| Elvaro Islami Muryadi received his bachelor’s degree in public health, Respati Indonesia University, Jakarta, Indonesia, in 2015. Prior to that, in 2023, he completed a master's program in public health at Prima Indonesia University, Medan, Indonesia, after completing a master's program in business administration at Respati Indonesia University, Jakarta, Indonesia, in 2018. At present, he is engaged in doctoral studies at Khon Kaen University, Thailand, Faculty of Medicine, Department of Community, Occupational, and Family Medicine. Health education, public health, health promotion, and family medicine are among his current research interests. Email: elvaroislamimuryadi.e@kkumail.com, Orcid: 0000-0001-5554-3641. |
|
|

| Dimas Chaerul Ekty Saputra received his bachelor’s degree from the Department of Informatics, Faculty of Industrial Technology, Ahmad Dahlan University, Yogyakarta, Indonesia in 2020, an M.Sc. degree in Department of Biomedical Engineering, Graduate School, Universitas Gadjah Mada, Yogyakarta, Indonesia in 2022, and now he is a PhD candidate in the Department of Computer Science, College of Computing, Khon Kaen University, Khon Kaen, Thailand. He is currently a lecturer at Telkom University Surabaya, Indonesia. He is also a member of the Association for Scientific Computing and Electronics, Engineering (ASCEE) Student Branch Indonesia. His research interests include artificial Intelligence, pattern recognition, machine learning, signal processing, and bioinformatics. Email: dimaschaerulekty@telkomuniversity.ac.id, Orcid: 0000-0001-6978-2846. |
Bibliometric Analysis of Explainable AI in Advance Care Planning: Insights, Collaborative Trends, and Future Prospects (Irianna Futri)